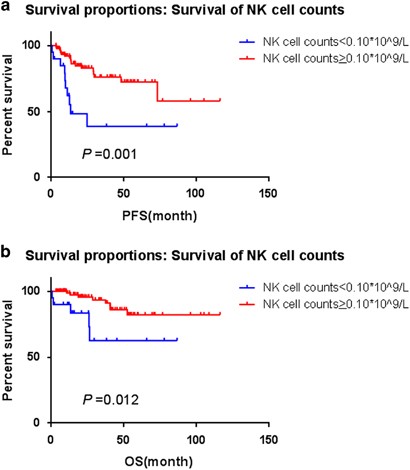
Low natural killer (NK) cell counts in peripheral blood adversely affect clinical outcome of patients with follicular lymphoma
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

The Follicular Lymphoma International Prognostic Index (FLIPI) and the Follicular Lymphoma International Prognostic Index-2 (FLIPI-2) have been widely used as models for predicting outcomes
in follicular lymphoma (FL) based on clinical parameters.1, 2 However, host immunity and tumor microenvironment are not taken into account by either FLIPI or FLIPI-2, which have been
demonstrated to remarkably influence the clinical outcomes of patients with FL. Thus, a series of studies have focused on the search for simple and effective surrogate biomarkers that are
immunologically relevant and can serve as prognostic factors.
Natural killer (NK) cells are important components of the innate immune response with crucial roles in eliminating viruses, regulating dendritic cells, and killing malignant cells.3 NK cell
count is a surrogate marker of host immune status. Previously, Plonquet et al.4 reported that the peripheral blood NK cell count was associated with clinical outcomes of diffuse large B-cell
lymphoma patients with age-adjusted International Prognostic Index scores of 2 or 3. To our knowledge, researches regarding prognostic value of peripheral blood NK cell counts in FL are not
very well established. Shafer et al.5 found that low NK cell counts in the blood (0.15 × 109/l) as suggested in earlier reports were associated with inferior OS by univariate analysis
(P=0.02) and trended toward significance by multivariate analysis (P=0.08). To reevaluate the role of NK cell counts in the prognosis of FL, we established this cohort study.
One hundred and thirty-two patients with FL were admitted to the First Affiliated Hospital of Nanjing Medical University, Jiangsu Province Hospital between January 2001 and October 2015, but
five of them were lost to follow-up. The diagnostic criteria and clinical management strategies did not change much during the follow-up times. All cases were pathologically confirmed as FL
according to 2008 WHO classification. Complete blood cell (CBC) data were collected in the remaining 127 FL patients upon diagnosis following an informed consent. However, only 114
patients’ peripheral blood flow cytometry (PBFCM) records at diagnosis for NK cell markers were available. Therefore, we retrospectively reviewed these 114 patients in this study. The counts
of peripheral blood NK cells were calculated from the percentages obtained by flow cytometry. NK cells were referred to CD3-CD16+ and/or CD56+ lymphocytes.
Baseline clinical characteristics were totally available, including age, gender, pathological grade, the number of nodal sites involved, bulky lesion, bone marrow involvement, Ann Arbor
stage, B symptoms, serum lactate dehydrogenase (LDH) and serum beta-2 microglobulin (β2-MG) (Table 1a). The FLIPI and FLIPI-2 were used for prognostic stratification. High FLIPI scores (high
risk) or high FLIPI-2 scores (high risk) were denoted as score ⩾3. Among the patients, 97 (85.1%) cases were treated with rituximab-containing therapy, 9 cases (7.9%) with chemotherapy and
2 cases (1.7%) with radiotherapy. A watch and wait approach was performed at diagnosis for remaining cases (5.3%). CBC and PBFCM analysis indicated that the median NK cell counts at
diagnosis were 0.17 × 109/l (range, 0.03 × 109/l−5.08 × 109/l). All P-values represented were two-sided, and statistical significance was declared at P