Intramedullary spinal cord abscess involving actinomyces and streptococcus: a case report and literature review
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT INTRODUCTION Intramedullary spinal cord abscesses (ISCA) are rare and caused by central nervous system infections. Although polymicrobial infections are rarely seen in ISCAs,
isolation of the causative pathogen is important for treatment. Here, we describe a very rare case of ISCA resulting from a mixed _Streptococcus_ and _Actinomyces_ infection. CASE
PRESENTATION An 82-year-old man presented with acute posterior cervical pain and progressive quadriplegia. Radiological investigations revealed a mass lesion showing marginal enhancement at
the level of the C3-4 vertebrae. Microsurgical drainage was performed, and _Streptococcus_ and _Actinomyces_ were identified as causative agents. Subsequent antibiotic treatment was noted to
be beneficial to the patient. DISCUSSION This case suggests that mixed infection can develop into ISCA depending on the causative agents such as _Actinomyces_. Prompt pathogen-directed
antibacterial therapy is required for ISCA treatment. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS SKIP DECOMPRESSION
SURGERIES IN THE TREATMENT OF HOLOSPINAL EPIDURAL ABSCESS: A CASE REPORT Article 13 May 2021 AN INFECTED ANDERSSON LESION PRESENTED WITH INCOMPLETE PARAPLEGIA IN A PATIENT WITH ANKYLOSING
SPONDYLITIS. A UNIQUE CASE REPORT WITH LITERATURE REVIEW Article 09 August 2022 SPINAL CORD DISORDER DUE TO SPINAL EPIDURAL ABSCESS SECONDARY TO THORACIC FACET JOINT SEPTIC ARTHRITIS—A RARE
CASE WITH A SURPRISING EVOLUTION Article 19 November 2020 INTRODUCTION Intramedullary spinal cord abscesses (ISCA) are rare and caused by central nervous system infections [1]. Although the
mortality rate improved to 8% between 1977 and 1997 due to advances made in pharmacology and radiology [1], ISCA remains intractable and has the potential to cause persistent neurological
deficits [1]. Therefore, early diagnosis and prompt treatment are key [2]. Thus, identification of the causative agent is important; however, culture and sensitivity tests can be
unsuccessful, depending on the agents [3]. Here, we describe a very rare case of ISCA due to mixed infection with _Streptococcus_ and _Actinomyces spp_., which was detected using cultures,
in conjunction with histopathological examinations. Adequate infection control was achieved by means of microsurgical drainage followed by prompt administration of antibiotic therapy. CASE
PRESENTATION An 82-year-old man presented with acute posterior cervical pain. He also demonstrated rapidly deteriorating paralysis (left>right) and was admitted to our hospital. He was
undergoing treatment for diabetes (HbA1c: 8.3%). Severe left and right-sided paralysis were observed. We assessed muscle strength with reference to the ASIA/ISCoS International Standards for
Neurological Classification of Spinal Cord Injury (ISNCSCI) [4]. Muscle function grading of key muscles was as follows (right/ left): elbow flexors, 3/1; wrist extensors, 3/1; elbow
extensors, 3/1; finger flexors, 3/1; finger abductors, 3/1; hip flexor, 3/1; knee extensors, 3/1; ankle dorsiflexors, 3/2; long toe extensors, 3/2; and ankle plantar flexors, 3/2. The motor
subscores were recorded as: upper extremity right, 15; upper extremity left, 5; upper extremity motor score, 20; lower extremity right, 15; lower extremity left, 8; lower extremity motor
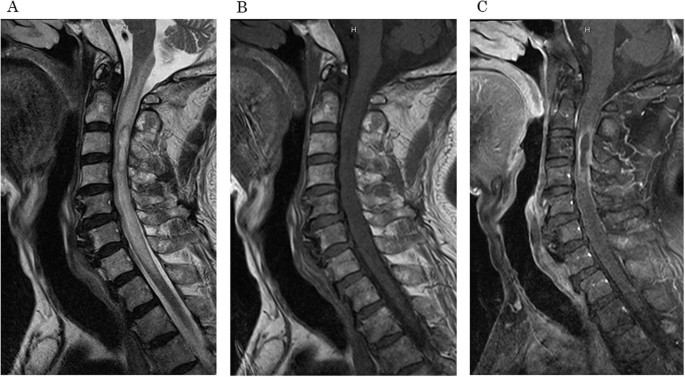
score, 23. ASIA Impairment Scale (AIS) was D. Magnetic resonance imaging (MRI) revealed a mass lesion with high intensity on T2-weighted images, low intensity on T1-weighted images, and
marginal enhancement at the level of C3-4 vertebrae (Fig. 1). Hematological examination revealed a white blood cell count of 12600/µl and a serum C-reactive protein level of 0.76 mg/dl.
Progressive quadriplegia and bladder-bowel dysfunction were observed, and emergency surgery was performed. Bilateral partial laminectomy at C2 and laminectomy at C3 and C4 were performed.
Following incision of the dura, the left dorsal side of the spinal cord was observed to be swollen at C4 (Fig. 2A). Myelotomy was performed at the abnormal left dorsal surface of the spinal
cord, and a milky white fluid resembling pus was drained (Fig. 2B). After abscess drainage and washing out of the cavity, the spinal cord swelling reduced (Fig. 2C). After surgery,
_Streptococcus constellatus_, which was Gram-positive coccus, was identified through culture of the abscess. In addition, histopathological examination identified a filamentous bacterial
mass with inflammatory cells, which was suspected to be _Actinomyces spp_. based on staining (positive Gram, negative Ziehl-Neelsen, and characteristic Grocott-Gomori) (Fig. 3). These
findings taken in conjunction suggest that the patient’s intramedullary spinal abscess was due to a mixed infection of _Streptococcus constellatus_ and _Actinomyces spp_. The administered
antibiotic therapy consisted of sulbactam/ampicillin for 8 weeks, followed by oral amoxicillin. Although no primary active sites of infection were detected, decayed teeth and chronic
periodontitis were observed. The abscess cavity as well as spinal cord edema improved (Fig. 4). He was transferred to a convalescent rehabilitation ward on postoperative day 69. The results
of muscle function grading of key muscles (right/ left) at the time of transfer were as follows: trapezius, 5/5; shoulder abductors, 4/4; elbow flexors, 4/3; wrist extensors, 4/2; elbow
extensors, 4/3; finger flexors, 3/3; finger abductors, 3/2; hip flexor, 3/1; knee extensors, 3/1; ankle dorsiflexors, 3/3; long toe extensors, 3/2; and ankle plantar flexors, 3/2. The
patient required severe assistance with transfer, bathing, toileting (needed urinary catheters), and ambulation. Through rehabilitation, the muscle strength of his upper extremities was
improved. He was able to transfer by himself and returned home 6 months postoperatively. His activities of daily living were preserved until 10 months postoperatively. The muscle function
grading result (right/ left) concerning elbow flexors, wrist extensors, elbow extensors and wrist flexors were all 5/5. Manual dexterity disorder of both hands remained mainly on the left
side. The lower extremities were mostly 4/2 on the muscle function grading (right/ left). Bladder-bowel dysfunction was not improved and, therefore, the urinary catheter could not be
removed. DISCUSSION We encountered a very rare case of intramedullary spinal cord abscess (ISCA), which itself is a rare central nervous system lesion, caused by a mixed infection of
_Streptococcus constellatus_ and _Actinomyces spp_ [1]. In 2020, Akimoto et al. reviewed approximately 150 cases of ISCA that have been reported in literature [5]. Previously, between 1830
and 1944, the mortality rate of ISCA cases was high (90%) [1]. With the development of antibacterial pharmacology and radiography, the mortality rate was improved [1]. However, ISCA remains
intractable because it can result in persistent neurological deficits [1]. Therefore, early diagnosis and prompt treatment are needed [2]. In this discussion, we review characteristics of
this disease that may aid in early diagnosis. First, clinical symptoms were analyzed. ISCA can present with progressive dorsal pain followed by acute neurological symptoms [6]. The symptoms
can progress rapidly and result in permanent neurological deficits [6]. In our case, quadriplegia occurred acutely and progressed over a period of hours. Secondly, characteristic features
facilitating radiographic diagnosis were reviewed. Contrast-enhanced T1-weighted MRI revealed a mass with a nodular-enhancing rim [7]. In addition, diffusion-weighted images showed
high-intensity signals in abscesses [7]. MRI features are useful in distinguishing ISCA from other acutely presenting intramedullary lesions, such as angioma. Appropriate antimicrobial
therapy is also integral in the management of this condition. Hence, identification of causative agents and routes of infection is key. Although ISCA can develop following the spread of a
primary infection, no other source is often detected [6]. Immunosuppressive conditions, such as diabetes, HIV infection, and steroid use, are potential risk factors for the development of
ISCA [8]. In addition, transient bacteremia from an odontogenic source could result in cryptogenic ISCA as well as brain abscesses [1]. The most frequent causative agent of ISCA is
_Staphylococcus_, followed by _Streptococcus_, _E. coli_, _Proteus_, _Listeria_, _Bacteroides_, _Pseudomonas_, _Brucella_, _Histoplasma_, _Toxoplasma_, and _Mycobacterium_ [2]. Polymicrobial
infections are rare in cases of ISCA [1]. To the best of our knowledge, we present the first reported case of ISCA due to mixed infection with _Streptococcus_ and _Actinomyces_.
_Actinomyces spp_. are facultatively anaerobic, branching gram-positive, acid-fast-negative bacilli [9]. They are found amidst the normal flora of the oropharyngeal cavity [9]. Abscess
formation, tissue fibrosis, and draining sinuses are characteristic of actinomycosis [9]. The most frequent site of infection is in the cervicofacial tissues. Actinomycosis involvement of
the central nervous system and spine is rare [3, 9]. _Actinomyces spp_. are frequently detected along with other bacteria, such as _Fusobacterium spp_., _Bacteroides spp_., _Capnocytophaga
spp_., _Eikenella spp_., _Staphylococcus spp_., _Streptococcus spp_., and _Enterococcus spp_ [10]. In ISCAs, _Actinomyces_ infection, including mixed infection, is extremely rare [11, 12].
Central nervous system actinomycosis is diagnosed on histopathological examination because culture is often inconclusive [3]. In the present case, _Actinomyces_ were not detected on culture,
although it was detected via histopathological examination. Thus, _Actinomyces_ might have the potential to cause ISCA, including a mixed infection as the root cause, and the detection of
_Actinomyces_ might have been difficult in previously reported cases. Although there are no treatment guidelines for ISCA, antimicrobial therapy is recommended for the management of
actinomycosis. Because premature antimicrobial therapy can result in relapse, 6–8 weeks of intravenous antimicrobial treatment, followed by 6–12 months of oral antimicrobial therapy is
recommended [10]. In conclusion, this case report suggests that mixed infection involving _Actinomyces spp_. has the potential to result in ISCA. In addition to culture and sensitivity
analyses, pathological examination of samples from the abscess could be useful in the detection of mixed infections, especially if _Actinomyces spp_. are involved, which may lead to prompt
antibiotic therapy. Prompt diagnosis and initiation of treatment were key factors that helped reduce the symptoms in the case reported. DATA AVAILABILITY The authors state that data
pertaining to this case report will be made available upon request. REFERENCES * Chan CT, Gold WL. Intramedullary abscess of the spinal cord in the antibiotic era: clinical features,
microbial etiologies, trends in pathogenesis, and outcomes. Clin Infect Dis. 1998;27:619–26. Article CAS PubMed Google Scholar * Sinha P, Parekh T, Pal D. Intramedullary abscess of the
upper cervical spinal cord. Unusual presentation and dilemmas of management: case report. Clin Neurol Neurosurg. 2013;115:1845–50. Article PubMed Google Scholar * Ravindra N, Sadashiva N,
Mahadevan A, Bhat DI, Saini J. Central nervous system actinomycosis—a clinicoradiologic and histopathologic analysis. World Neurosurg. 2018;116:e362–70. Article PubMed Google Scholar *
Kirshblum S, Snider B, Rupp R, Read MS. International Standards Committee of ASIA and ISCoS. Updates of the international standards for neurologic classification of spinal cord injury: 2015
and 2019. Phys Med Rehabil Clin N. Am. 2020;31:319–30. Article PubMed Google Scholar * Akimoto T, Hirose S, Mizoguchi T, Yokota Y, Hara M, Ishihara M, et al. Ruptured long intramedullary
spinal cord abscess successfully treated with antibiotic treatment. J Clin Neurosci. 2020;82:249–51. Article CAS PubMed Google Scholar * Cerecedo-Lopez CD, Bernstock JD, Dmytriw AA, Chen
JA, Chalif JI, Gupta S, et al. Spontaneous intramedullary abscesses caused by Streptococcus anginosus: two case reports and review of the literature. BMC Infect Dis. 2022;22:141. Article
PubMed PubMed Central Google Scholar * Bakhsheshian J, Kim PE, Attenello FJ. Intramedullary cervical spinal cord abscess. World Neurosurg. 2017;106:1049.e1–e2. Article PubMed Google
Scholar * Keefe P, Das JM, Al-Dhahir MA. Spinal Cord Abscess, in StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC., 2022. * Duvignaud A,
Ribeiro E, Moynet D, Longy-Boursier M, Malvy D. Cervical spondylitis and spinal abscess due to Actinomyces meyeri. Braz J Infect Dis. 2014;18:106–9. Article PubMed Google Scholar * Honda
H, Bankowski MJ, Kajioka EH, Chokrungvaranon N, Kim W, Gallacher ST. Thoracic vertebral actinomycosis: actinomyces Israelii and Fusobacterium nucleatum. J Clin Microbiol. 2008;46:2009–14.
Article CAS PubMed PubMed Central Google Scholar * David C, Brasme L, Peruzzi P, Bertault R, Vinsonneau M, Ingrand D. Intramedullary abscess of the spinal cord in a patient with a
right-to-left shunt: case report. Clin Infect Dis. 1997;24:89–90. Article CAS PubMed Google Scholar * Simon JK, Lazareff JA, Diament MJ, Kennedy WA. Intramedullary abscess of the spinal
cord in children: a case report and review of the literature. Pediatr Infect Dis J. 2003;22:186–92. Article PubMed Google Scholar Download references AUTHOR INFORMATION AUTHORS AND
AFFILIATIONS * Department of Neurosurgery, Gunma University Graduate School of Medicine, Maebashi, Gunma, Japan Shunsuke Nakamura, Hiroya Shimauchi-Ohtaki, Fumiaki Honda & Yuhei
Yoshimoto * Infection Control and Prevention Center, Gunma University Hospital, Maebashi, Gunma, Japan Yutaka Tokue Authors * Shunsuke Nakamura View author publications You can also search
for this author inPubMed Google Scholar * Hiroya Shimauchi-Ohtaki View author publications You can also search for this author inPubMed Google Scholar * Fumiaki Honda View author
publications You can also search for this author inPubMed Google Scholar * Yutaka Tokue View author publications You can also search for this author inPubMed Google Scholar * Yuhei Yoshimoto
View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS SN and HS were responsible for writing the report, conducting the literature search,
extracting and analyzing data, interpreting results, and updating reference lists. FH was responsible for extracting and analyzing data and interpreting results. YT and YY provided feedback
on the report. CORRESPONDING AUTHOR Correspondence to Hiroya Shimauchi-Ohtaki. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ETHICAL APPROVAL As this is
a case report, informed consent was obtained from the patient for publication, and institutional ethical review was deemed unnecessary. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer
Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS Springer Nature or its licensor (e.g. a society or other
partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this
article is solely governed by the terms of such publishing agreement and applicable law. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Nakamura, S., Shimauchi-Ohtaki, H.,
Honda, F. _et al._ Intramedullary spinal cord abscess involving _Actinomyces_ and _Streptococcus:_ a case report and literature review. _Spinal Cord Ser Cases_ 10, 6 (2024).
https://doi.org/10.1038/s41394-024-00618-5 Download citation * Received: 25 July 2022 * Revised: 06 February 2024 * Accepted: 08 February 2024 * Published: 17 February 2024 * DOI:
https://doi.org/10.1038/s41394-024-00618-5 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative