Lysates of Lactobacillus acidophilus combined with CTLA-4-blocking antibodies enhance antitumor immunity in a mouse colon cancer model
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

Previous reports have suggested that many gut microbiomes were associated with the development of colorectal cancer (CRC), and could modulate response to numerous forms of cancer therapy,
including checkpoint blockade immunotherapy. Here we evaluated the protective efficacy of Lactobacillus acidophilus (L. acidophilus) cell lysates combined with an anti-CTL antigen-4 blocking
antibody (CTLA-4 mAb) in syngeneic BALB/c mice CRC models induce by a single intraperitoneal injection of 10 mg/kg azoxymethane (AOM), followed by three cycles of 2% dextran sulfate sodium
(DSS) in drinking water. In contrast to CTLA-4 mAb monotherapy, L. acidophilus lysates could attenuate the loss of body weight and the combined administration significantly protected mice
against CRC development, which suggested that the lysates enhanced antitumor activity of CTLA-4 mAb in model mice. The enhanced efficacy was associated with the increased CD8 + T cell,
increased effector memory T cells (CD44 + CD8 + CD62L+), decreased Treg (CD4 + CD25 + Foxp3+) and M2 macrophages (F4/80 + CD206+) in the tumor microenvironment. In addition, our results
revealed that L. acidophilus lysates had an immunomodulatory effect through inhibition the M2 polarization and the IL-10 expressed levels of LPS-activated Raw264.7 macrophages. Finally, the
16S rRNA gene sequencing of fecal microbiota demonstrated that the combined administration significantly inhibited the abnormal increase in the relative abundance of proteobacteria and
partly counterbalance CRC-induced dysbiosis in model mice. Overall, these data support promising clinical possibilities of L. acidophilus lysates with CTLA-4 mAb in cancer patients and the
hypothesis that probiotics help shape the anticancer immune response.
Colorectal cancer (CRC) is the fourth leading cause of cancer-related death worldwide. The development of this disease may be attributed to numerous factors such as gene mutations, family
history, dietary composition, and inflammatory dysregulation1,2. Recently, valuable insights have been gained into the role of the intestinal microbiota in CRC development, and extensive
investigations have suggested that intestinal microbial homeostasis is closely related with above pathogenic factors of CRC3,4,5.
After birth, the microbiota of an individual is mainly shaped by maternal factors related to birthing and postnatal factors such as diet and environment6,7. These microbiota offer
nutritional, immune defense, and immune development-related development benefits to the host8,9. Microorganisms colonizing in the intestine are in a dynamic equilibrium10, and the
composition of the microbial community may be affected by alcohol consumption, diet, and the intestinal micro-environmental factors such as pH, mucosal integrity, and nutrient
availability11. Additionally, growing evidence shows that abnormal gut microbiota participate in various pathophysiological processes associated with many diseases, including CRC4,5.
However, the specific roles of each microbe in CRC development are unclear.
Previous studies have shown that some probiotic bacteria, such as Bifidobacterium longum12, Lactobacillus acidophilus13, and Enterococcus faecalis14, mediate inflammatory responses, inhibit
the proliferation of malignant cells, and reduce levels of pro-carcinogenic metabolites in CRC. Additionally, Aghazadeh et al. reported that the secretions of an Acetobacter syzygii strain
exerted anti-cancer effects against squamous cell carcinoma15.
Preliminary data have shown that probiotic lysates, unlike live microbes, may be administered therapeutically without potential adverse side effects, which are particularly oriented towards
immune system regulation16,17. Furthermore, the use of probiotic lysates would allow the manufacturers of probiotic products to circumvent the logistical challenges of maintaining the
viability of bacteria during formulation, transportation, and preservation18. The objective of the present study was to determine whether a combination of administered probiotic lysates and
checkpoint blockade could enhance antitumor immune responses. We evaluated the efficacy of the lysate of L. acidophilus and anti-mouse (m) CTLA-4 antibodies, administrated alone or in
combination, in mouse CRC models chemically induced using azoxymethane (AOM) and dextran sodium sulfate (DSS).
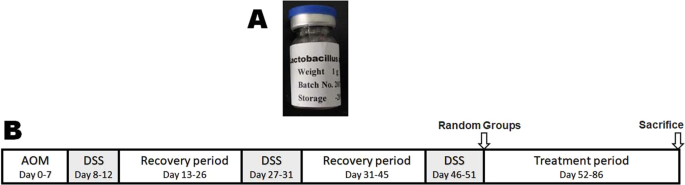
L. acidophilus (ATCC 33198) were purchased from China General Microbiological Culture Collection Center (CGMCC), Beijing, China, and were cultured in 10 L MRS broth at 37 °C. After 24 h, the
cells were harvested by centrifuging at 4,000 × g (4 °C and 20 min), washed with phosphate-buffered saline (PBS) three times. Then, the cell pellet was re-suspended in PBS at a
concentration of 108 CFU/ml, and disrupted at 1,200 bar (4 °C, 2 min/time, 3 times) with JN-6000C PLUS low-temperature ultrahigh-pressure continuous flow cell crusher (JNBIO, Guangzhou,
China)19. Finally, after centrifuged at 4,000 × g (4 °C and 20 min) to remove any whole bacteria remaining, the lysate of L. acidophilus was freeze-dried in a bottle (Fig. 1A). Before
intragastric administration (i.g.), the freeze-dried lysates were dissolved in ddH2O at a concentration of 108 CFU/ml.
Schematic time schedule of combination therapy with anti–CTLA-4 antibodies and probiotic lysates (A) Lysates of Lactobacillus acidophilus. (B) Experimental protocol for the induction of
colorectal cancer and combination therapy in BALB/c mice. A single intraperitoneal injection of 10 mg/kg azoxymethane (AOM) at 7 days was followed by three cycles of administration of 2%
dextran sulfate sodium (DSS) in sterile drinking water for 5 days, followed by normal drinking water for another 14 days. Then, the following two experiments were performed. Experiment 1#
(Lysates therapy every other day from day 52), Low-dose group (i.g., lysates of 5 × 106 CFU L. acidophilus/mouse); High-dose group (i.g., lysates of 2 × 107 CFU L. acidophilus/mouse) and PBS
control group (i.g., equivalent volume PBS). Experiment 2# (Combined therapy every other day from day 52), CTLA-4 IgG group (50 μg/mouse); Lysates group (i.g., lysates of 5 × 106 CFU L.
acidophilus/mouse); Combined group (50 μg/mouse i.p. and the equivalent lysates i.g.); Model control group (equivalent volume PBS, i.p. and i.g.) and Normal control group (equivalent volume
of PBS, i.p. and i.g.).
All experiments were performed in accordance with institutional ethical guidelines, and the study was approved by the Ethics Committee for Animal Research of Nanjing Medical University.
Healthy male BALB/c mice (6–8 weeks old) were obtained from the Model Animal Research Center of Nanjing University (Nanjing, China) and housed in specific pathogen-free conditions at Nanjing
First Hospital Animal Center, Nanjing, China, in a room controlled for temperature (21 ± 2 °C), humidity (55 ± 5%), and light (12-h light/dark cycle).
For generating colitis-associated CRC models, mice (with the exception of normal negative control) were induced with a single intraperitoneal injection of 10 mg/kg azoxymethane (AOM)
(Sigma-Aldrich, St. Louis, MO) 7 days, and subsequently induced by three cycles of 2% dextran sulfate sodium (DSS) (MP Biomedicals, Santa Ana, CA) in sterile drinking water for 5 days,
followed by normal drinking water for another 14 days (Fig. 1B), as previously described20. On day 52, the induced mice were randomly assigned to different groups (n = 10/group) as
following.
Mice were administrated by lysates every other day for 5 weeks as follows: low-dose group (i.g., lysates of 5 × 106 CFU L. acidophilus/mouse), high-dose group (i.g., lysates of 2 × 107 CFU
L. acidophilus/mouse) and PBS control (i.g., equivalent volume PBS).
Mice then received combined therapy every other day for 5 weeks as follows: CTLA-4 IgG group (anti-mouse-CTLA-4 IgG in PBS, clone# 9H10, intraperitoneal injection i.p., 50 μg/mouse)21;
lysates group (i.g., lysates of 5 × 106 CFU L. acidophilus/mouse); combined group, (equivalent dose anti-CTLA-4 IgG i.p. and lysates i.g.) and model control group (equivalent volume PBS,
i.p. and i.g.). The mice in the normal control group were also treated with an equivalent volume of PBS, i.p. and i.g.
A 4-week study was conducted in male BALB/c mice to evaluate the toxicity of administered lysate of L. acidophilus. The study-specific protocol was approved by the Ethics Committee for
Animal Research of Nanjing Medical University. Thirty mice were randomized into 3 groups (n = 6/group): Low does lysates (i.g., lysates of 5 × 106 CFU L. acidophilus), High does lysates
(i.g., lysates of 2 × 107 CFU/ml. acidophilus), or PBS control group (i.g., 200 μl/mouse PBS). After receiving an intragastric administration once a day for 28 days, the mice were evaluated
for changes in clinical signs daily and body weights were recorded weekly. After the last lysate dose, all mice were euthanized by CO2 inhalation on day 29. Colorectal tissues were processed
for microscopic and histologic evaluations, and lymphocyte subsets in peripheral blood and mesenteric lymph nodes were analysed by flow cytometry on day 29.
Body weights were monitored weekly over the duration of the experiment. Symptom severity was assessed twice/week beginning at the first cycle of DSS exposure, by symptom score as previously
described22, which included body weight loss (WL) (0 = 15%); stool consistency (0 = pellet, 2 = pasty, and 4 = diarrhea); occult/gross rectal bleeding assessed by the urine fecal occult
blood test kit (Shanghai Yisheng Biological Technology Co., Ltd.) (0 = negative, 2 = positive, and 4 = gross bleeding). Mice were sacrificed at day 85. Colons tissues were collected, cleaned
with PBS, and stored under required conditions for subsequent analyses.
Whole-colon tissues were thoroughly rinsed and then fixed in 10% formalin for 24 hours. After each group of colon tissues was embedded together with a paraffin block, the fixed tissues were
sectioned and stained by hematoxylin/eosin (H&E) staining and immunohistochemical staining with primary rabbit anti-mouse CD8a (Cell Signaling Technology, #98941, 1:400), rabbit anti-mouse
Foxp3 (Cell Signaling Technology, #12653, 1:100), or rabbit anti-mouse Granzyme B (Cell Signaling Technology, #46890, 1:125), and then anti- rabbit IgG-HRP secondary antibodies. Finally, a
pathologist who was blinded to the clinical data for all mice evaluated all sections for numbers of tumors and immunohistochemical staining of whole-colon tissues.
The cytokine mRNA levels in peritoneal macrophages and mesenteric lymph nodes were analyzed by quantitative real-time PCR (qRT-PCR), as previously described. Briefly, primary peritoneal
macrophages were isolated from the sacrificed mice at day 85 by injecting their peritoneal cavity with 10 ml of Dulbecco’s modified Eagle’s medium (DMEM), massaging, and then drawing back to
the syringe the fluid now containing the macrophages. After centrifugation, cells were resuspended in DMEM with 10% fetal bovine serum (FBS) (Gibco, Life Technologies, USA) and 1% v/v
penicillin and streptomycin (Gibco, Life Technologies, USA), and were plated 6-well plates for 2 h to facilitate adherence at 37 °C in a 5% CO2 incubator. The adherent cells, regarded as
primary peritoneal macrophages, were analyzed the cytokine mRNA levels by qRT-PCR.
The qRT-PCR was performed in both the peritoneal macrophages and mesenteric lymph node tissue following RNA isolation with TRIzol reagent (Invitrogen Life Technologies, Paisley, UK). The
cDNA template was synthesized using a HiScript® 1st Strand cDNA Synthesis kit (Vazyme Biotech Co., Ltd, Nanjing, China); then, qPCR analysis was performed using a AceQ Universal SYBR Green
qPCR Master Mix (Vazyme Biotech Co., Ltd, Nanjing, China), according to standard protocols, using TNF-α, IL-2, IL-10, and IFN-γ primers. Relative gene expression was normalized to the
expression of actin. All primer sequences are shown in Table S4.
We assessed lymphocyte subsets from the mesenteric lymph node samples by flow cytometry. Briefly, single cell suspensions were prepared by smashing Peyer’s patches and mesenteric lymph node
tissues with a syringe and nylon mesh, and washing with PBS. Then, we stained the cells (100 μL) with the different antibody panels at working concentrations as follows: FITC Rat Anti-Mouse
CD4 (Clone# H129.19), PE-Cy™5 Rat Anti-Mouse CD8a (Clone# 53–6.7), APC anti-Mouse Foxp3 (Clone# 3G3), PE Rat Anti-Mouse CD25 (Clone# PC61), FITC Rat Anti-Mouse CD44 (Clone# IM7), PE-Cyanine7
anti-mouse IFN-γ (Clone# XMG1.2) and PE-Cyanine7 anti-mouse CD62L (Clone#MEL-14). Additionally, peritoneal macrophages were collected from mice injected with 5 mL of PBS and stained with
the panel of PerCP-Cyanine5.5 anti- mouse F4/80 (Clone# BM8), PE anti-mouse CD206 (Clone#MR6F3) and FITC anti-mouse CD11b (Clone#M1/70). After incubation in the dark at 4 °C for 20 min and
washing twice in PBS, the stained cells were analyzed using a FACSCanto™ II flow cytometer (BD Biosciences, San Diego, CA, USA). Finally, the data were analyzed using FlowJo software
(Treestar, San Carlos, CA, USA).
After aseptic collection from each mouse, the feces were kept in sterile tubes and immediately frozen at −80 °C for microbial DNA extraction and analysis of bacterial community composition.
Briefly, PCR products were amplified from the V4-V5 regions of the bacterial 16S ribosomal RNA gene using primers of 27 F (AGAGTTTGATCCTGGCTCAG) and 533 R (TTACCGCGGCTGCTGGCAC), purified
using the AxyPrep DNA Gel Extraction Kit (Axygen Biosciences, Union City, CA, USA from 2% agarose gels, and then paired-end sequenced on an Illumina MiSeq platform (Majorbio Biomedical
Technology Co., Ltd, Shanghai, China) according to standard protocols. Finally, all sequence data were analyzed by the Ribosomal Database Project (RDP) Classifier against the Silva 16S rRNA
database (SSU117) with a confidence threshold of 70%23.
The macrophage RAW 264.7 cell line (purchased from Shanghai Cell Bank, Chinese Academy of Sciences) were cultured in complete Dulbecco’s modified Eagle’s medium (DMEM) (Gibco, Carlsbad, CA)
with 10% fetal bovine serum (FBS) (Gibco) and 1% v/v penicillin and streptomycin (Gibco) at 37 °C in a 5% CO2 incubator. Briefly, the cells were cultivated in the presence of different
protein concentrations of bacterial lysate (filtered by the 0.22 micron membrane), or sterile PBS in the presence or absence of 1 μg/ml lipopolysaccharide (LPS, Sigma-Aldrich). After
cultivation 24 h, we analyzed the mRNA levels of tumour necrosis factor α (TNF-α) and IL-10 by qRT-PCR and the CD206 (macrophage mannose receptor) expressed levels of RAW264.7 cells by flow
cytometric analysis.
Data were analyzed with GraphPad Prism version 5 (San Diego, CA, USA). Two-tailed Student’s t-tests were used to compare experimental groups. Statistical significance was defined at greater
than or equal to a 95% confidence interval or a p-value