The expression and clinical significance of programmed cell death receptor 1 and its ligand in tumor tissues of patients with extranodal nasal nk/t cell lymphoma
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT Appropriate biomarkers may help distinguish the biological behavior of different types of lymphoma and their response to traditional chemotherapy. Extranodal natural killer/T-cell
lymphoma (ENKTL) and diffuse large B-cell lymphoma (DLBCL) belong to different subtypes of non-Hodgkin's lymphoma, the biological behavior and prognosis of them are very different,
programmed cell death receptor 1 (PD-1) and its ligand (PD-L1) have been investigated in these two types of diseases. However, few studies addressed the difference of PD-1/PD-L1 levels
between ENKTL and DLBCL, in order to find out the difference and related clinical application value, the clinical data and tumor tissue paraffin sections of 24 newly diagnosed ENKTL patients
and 42 newly diagnosed diffuse large B-cell lymphoma (DLBCL) were collected. PD-1/PD-L1 levels in tumor tissues were detected by immunohistochemical staining. The relationship between the
PD-1/PD-L1 levels and clinical data of patients with ENKTL patients was analyzed. Both patient groups showed PD-1 level in tumor tissue of ENKTL patients was significantly lower than that of
DLBCL patients (P < 0.05), while the PD-L1 level in tumor tissues of ENKTL patients was not different from DLBCL (P < 0.05). In addition, the ENKTL patients with B symptoms, elevated
lactate dehydrogenase (LDH) levels and decreased hemoglobin (HGB) concentrations had lower level of PD-1 in tumor tissue. PD-L1 level in tumor tissues, the LDH level, Epstein-Barr genome
(EBV-DNA) copy and Ki-67 index may affect the outcomes of ENKTL patients (P < 0.05), but they were not independent factors. PD-L1 levels in tumor tissues has clinical significance in
ENKTL patients, which suggested that the PD-1/PD-L1 signal pathway may be involved in the immune escape of ENKTL and play different roles in different lymphoma subtypes. SIMILAR CONTENT
BEING VIEWED BY OTHERS INCREASED COEXPRESSION OF PD-L1 AND IDO1 IS ASSOCIATED WITH POOR OVERALL SURVIVAL IN PATIENTS WITH NK/T-CELL LYMPHOMA Article 23 May 2024 A RETROSPECTIVE STUDY ON THE
CLINICOPATHOLOGICAL AND MOLECULAR FEATURES OF 22 CASES OF NATURAL KILLER/T-CELL LYMPHOMA IN CHILDREN AND ADOLESCENTS Article Open access 03 May 2022 IMPROVED PROGNOSIS OF ADVANCED-STAGE
EXTRANODAL NK/T-CELL LYMPHOMA: RESULTS OF THE NKEA-NEXT STUDY Article Open access 17 February 2025 INTRODUCTION Extranodal NK/T-cell lymphoma, nasal type (ENKTL) is an aggressive non-Hodgkin
lymphoma which originates from T cell or NK-like cell, it often involve the nasal cavity, face and upper respiratory tract. Compared to diffuse large B-cell lymphoma (DLBCL), this disease
is characterized by more difficult diagnosis, higher malignant, rapider progress, and easier to be resistant to traditional chemotherapy. Therefore, there is currently no standard treatment
plan for ENKTL1. The above characteristics are probably related to tumor cells evading the immune response of the body, the signaling pathway involving programmed cell death receptor 1
(PD-1) is likely one mechanisms of immune evasion2,3. Existing studies have shown that PD-1 is mainly expressed on CD4+ or CD8+ T cell membranes, and it has two types of ligands, which are
PD-L1 and PD-L2. PD-L1 is the main ligand of PD-1 in the human body, PD-L1 is expressed in not only immune cells such as activated lymphocytes, NK cells and macrophages, but also tissue
cells such as lung and vascular endothelium2. What is more, it is expressed at high levels in tumor cells, such as melanoma4, gastric cancer5, kidney cancer6, high levels of PD-L1 expressed
on tumor cells can inhibit the proliferation and activation of lymphocytes by interacting with PD-1 on lymphocytes to achieve the immune escape of tumor cells2. Recent studies have shown
that PD-L1 level in nasal biopsy tissues of ENKTL patients is much higher than that of rhinitis patients7. At present, the clinical trials of PD-1 monoclonal antibody are already underway.
PD-1 monoclonal antibody has achieved very good outcomes in ENKTL8, but it didn’t achieve good outcomes in DLBCL9. Therefore, we hope to explore the reasons by comparing the expression
differences of PD-1/PD-L1 level in these two diseases. Based on the above background, we used a retrospective case–control study to analyze the differences in PD-1/PD-L1 levels in tumor
tissues of between ENKTL and DLBCL patients. Therefore we examined PD-1/PD-L1 in tumor tissues of ENKTL and DLBCL patients. Our results show that PD-1/PD-L1 level in tumor tissues of ENKTL
patients are useful for staging and prediction of treatment response in ENKTL. The same results were not obtained for patients with DLBCL, another type of lymphoma, suggesting that the
biomarker may show some clinical significance for ENKTL. MATERIALS AND METHODS STUDY POPULATION AND TREATMENT This retrospective study included 24 cases of ENKTL (18 males, median age 49.5
years) diagnosed in West China Hospital of Sichuan University from December 2017 to December 2018 and 42 cases of DLBCL patients, and pathological paraffin sections of all 66 patients have
been obtained from the Department of Pathology, West China Hospital, Sichuan University. The diagnostic criteria are based on the 2008 WHO classification criteria for hematopoietic and
lymphoid tissue tumors10. The outcomes evaluation after two courses of chemotherapy follows the "Evaluation Criteria for the outcomes of Malignant Lymphoma", including complete
remission (CR), partial remission (PR), stable disease (SD) and disease progression (PD)11. We have signed an informed consent form with all research subjects, and have been approved by the
Ethics Committee of West China Hospital of Sichuan University. All methods are performed in accordance with the relevant guidelines and regulations. IMMUNOHISTOCHEMICAL STAINING (IHC) FOR
PD-1/PD-L1 Paraffin-embedded sections (3 µm) were used for immunohistochemical staining (IHC). After being dewaxed and hydrated, antigen retrieval (citric acid with PH = 9) and inactivation
of endogenous peroxidase, the primary antibody [PD-L1 antibody [28-8] (Abcam, Cambridge, UK)/PD-1 antibody (Zhongshan Jinqiao, Beijing, China), dilution 1:75] and general secondary antibody
for antibody incubation, after washing with running water, DAB is added dropwise to develop color, after the color is developed, hematoxylin counterstaining is carried out, and then
dehydrated and mounted. Observe the slices under a microscope and collect images, IHC was accomplished by avidin–biotin peroxidase complex detection system. The percentage of PD-1/PD-L1
expression (the number of cells stained with membranes in the total number of tumor cells) was analyzed by Image J software. The percentage > 30% was defined as PD-L1 (+), while the
percentage > 5% was considered PD-1 (+)12. STATISTICAL ANALYSES PD-1/PD-L1 level in tumor tissues are presented as the median and interquartile range [M(IQR)]. The Kruskal–Wallis test was
used to analyze the differences between groups, and the Mann–Whitney U test and Spearman rank correlation analysis were used to analyze the relationship between PD-1/PD-L1 level in tumor
and the clinical data of patients. Fish test and Logistic regression were used to conduct univariate and multivariate analysis of predictors of treatment response in ENKTL patients. We set P
value < 0.05 as the significant difference. ETHICS APPROVAL AND CONSENT TO PARTICIPATE This study was approved by the Ethics Committee of West China Hospital of Sichuan University.
Participants provided written consent for their anonymized clinical data to be used and published for research purposes. RESULTS BASELINE CLINICAL CHARACTERISTICS OF PATIENTS Baseline
clinical characteristics of 24 patients with ENKTL and 42 ones with DLBCL are summarized in Table 1. In the ENKTL group, 7 (29%) was in stage III-IV, and 8 (33%) had LDH > 250 U/L. 23
(88%) patients accepted anthracycline-containing chemotherapy regimens. All patients received at least two cycles of chemotherapy before radiotherapy. After two courses of chemotherapy, 8
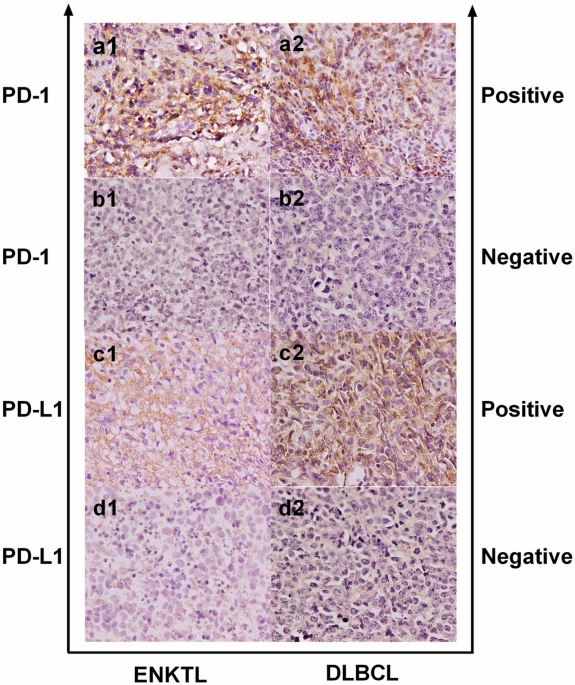
patients (33%) achieved CR. PD-1 AND PD-L1 LEVELS IN TUMOR TISSUES AND RELATIONSHIPS WITH CLINICAL VARIABLES The distribution and expression of PD-1/PD-L1 in tumor tissues were investigated
by immunohistochemical staining. Membranes of positive cells in tumor tissues from ENKTL and DLBCL patients were stained brown (Fig. 1). PD-L1 (+) was defined as positive cells proportion
> 30% and PD-1 (+) as > 5%12. In 24 ENKTL patients, 19 (79%) were PD-L1 (+) and 9 (38%) were PD-1(+) (Fig. 2A). In 42 DLBCL patients, 25 (60%) were PD-L1 (+) and 29 (69%) were PD-1 (+)
(Fig. 2B). PD-1 level in tumor tissues in ENKTL patients [3.50(0.00–9.75)] was significantly lower than in DLBCL patients [21.00(1.75–44.00), P = 0.0021] (Fig. 2C), while PD-L1 level was
not statistically different between ENKTL [49.50(35.25–80.00)] and DLBCL [50.50(2.50–77.00)] groups (Fig. 2D). In ENKTL patients, PD-1 level in tumor tissues were significantly lower with B
symptoms#, higher levels of LDH (P < 0.05, Fig. 3A), and lower hemoglobin level (Spearman r = 0.6131, P = 0.0014, Fig. 3B). ASSOCIATION OF PD-1 OR PD-L1 BIOMARKERS WITH TREATMENT RESPONSE
As shown in Table 2, Univariate analysis showed that ENKTL patients with higher levels of PD-L1 in tumor tissues (P = 0.0218) were more difficult to achieve CR, as were patients with high
levels of LDH (P = 0.0222), Ki-67 index (P = 0.0304) and EBV-DNA copies (P = 0.0087). In multivariate analysis, the covariates we chose are LDH, EBV-DNA copies, Ki-67 index, PD-L1 level in
tumor tissues, however, no one varied significantly with treatment response. CORRELATION AMONG PD-1/PD-L1 LEVEL IN TUMOR TISSUES, PD-L1MRNA LEVEL IN PBMCS AND SPD-L1 LEVEL Early research by
our research group detected expressions of PD-1/PD-L1 in peripheral blood mononuclear cells (PBMCs) and plasma. We used the same cohort of patients as before, however, pathological specimens
of some patients are not available, so the number of patients included in this article has decreased. We made a correlation analysis of PD-1/PD-L1 level between tumor tissue and peripheral
blood, our results showed PD-1 level in tissues was correlated with PD-L1mRNA level in PBMCs (P = 0.0109, Spearman r = − 0.5097, Fig. 4A) and sPD-L1 level (P = 0.0086, Spearman r = − 0.5237,
Fig. 4B), Unfortunately, we didn’t find a correlation between PD-L1 level in tumor tissues and soluble PD-L1 level in peripheral blood. DISCUSSION Studies have found that in patients with
follicular lymphoma, PD-1 is mainly expressed on CD4+ T lymphocytes in lymph node follicles13. Roncador G, García Verdes-Montenegro JF found that PD-1 is abnormally highly expressed in
tissues of patients with angioimmunoblastic lymphoma (AITL)14. Jo et al. have reported the low level of PD-1 in tumor tissues of ENKTL patients15, and Muhamad et al. also found that PD-1 was
positive in 20.5% of stroma, but undetectable on lymphoma cells16. Similarly, this study found that PD-1 level in tumor tissues of ENKTL patients was significantly lower than that of DLBCL
patients, and that PD-1 level in tumor tissues of ENKTL patients with B symptoms, increased LDH levels, and decreased hemoglobin concentration was lower. We believe that the low level of
PD-1(+) infiltrating lymphocytes constitutes the immunosuppressive effect of lymphoma cells in tumor microenvironment and promotes tumor immune escape, from this perspective, the lower PD-1
level in ENKTL tumor tissue may be one of the possible reasons why ENKTL progresses faster than DLBCL. In addition, Chen BJ, Chapuy B and other scholars have found that PD-L1 is expressed in
HL, DLBCL, ENKTL and other lymphoma tissues, but no expression has been detected in Burkitt lymphoma17, similar to this, this study is also found that PD-L1 is highly expressed in tumor
tissues of ENKTL and DLBCL patients, it is suggested that the increased expression of PD-L1 is one of the possible reasons for the defect of cellular immune function in patients. The
outcomes-related analysis in ENKTL patients found that the LDH level, EBV-DNA copy number, Ki-67 index and PD-L1 level in tumor tissues will affect the outcomes of ENKTL patients, but are
not independent factors. Li et al. also found that Persistent peripheral blood EBV-DNA positive with high expression of PD-L1 and upregulation of CD4 + CD25 + T cell ratio in early stage
NK/T cell lymphoma patients may predict worse outcome18. Similarly, we also found high levels of EBV-DNA copies were more difficult to achieve CR. Bi et al. found that Patients with a high
concentration of serum soluble PD-L1 or with a high percentage of PD-L1 expression in tumor specimens exhibited significantly lower response rate to treatment and remarkably worse survival,
compared with their counterparts19. Wang et al. also found that Patients with high pretreatment had shorter progression-free survival and overall survival20. However, Kim found that PD-L1
expression was the only significant independent predictor for longer OS in patients with advanced stage (III/IV) ENKTL21. For this contradictory result, We analyzed the patient staging of
three articles, We found that the patients studied in the first two articles are all classified as stage I–II patients, the third article was for patients with stage III–IV. We believed that
PD-L1-mediated inhibition may lead to local depletion of cytokines involved in the survival and growth of cancer cells, resulting in anti-tumor effects in patients with advanced stage
(III/IV) ENKTL, This also showed that PD-L1 played different roles in ENKTL patients of different stages. These suggest that the PD-1/PD-L1 signaling pathway may be involved in the disease
progression of ENKTL patients, and is closely related to the patient's response to traditional chemotherapy. In summary, the results of this study showed that the expression of
PD-1/PD-L1 in the tumor tissues of patients is different in ENKTL and DLBCL patients, suggesting that the PD-1/PD-L1 signaling pathway has different roles in different lymphoma subtypes.
DATA AVAILABILITY The datasets generated and analyzed in the current study are available from the corresponding author on reasonable request. REFERENCES * Kwong, Y. L. _et al._ CD56+ NK
lymphomas: Clinicopathological features and prognosis. _Br. J. Haematol._ 97(4), 821–829 (1997). Article CAS Google Scholar * Keir, M. E. _et al._ PD-1 and its ligands in tolerance and
immunity. _Annu. Rev. Immunol._ 26, 677–704 (2008). Article CAS Google Scholar * Rong, Q. X. _et al._ GM-CSF mediates immune evasion via upregulation of PD-L1 expression in extranodal
natural killer/T cell lymphoma. _Mol. Cancer_ 20(1), 80 (2021). Article CAS Google Scholar * Chen, G. _et al._ Exosomal PD-L1 contributes to immunosuppression and is associated with
anti-PD-1 response. _Nature_ 560(7718), 382–386 (2018). Article ADS CAS Google Scholar * Wu, C. _et al._ Immunohistochemical localization of programmed death-1 ligand-1 (PD-L1) in
gastric carcinoma and its clinical significance. _Acta Histochem._ 108(1), 19–24 (2006). Article Google Scholar * Thompson, R. H. _et al._ Tumor B7–H1 is associated with poor prognosis in
renal cell carcinoma patients with long-term follow-up. _Cancer Res._ 66(7), 3381–3385 (2006). Article CAS Google Scholar * Han, L. _et al._ Role of programmed death ligands in effective
T-cell interactions in extranodal natural killer/T-cell lymphoma. _Oncol. Lett._ 8(4), 1461–1469 (2014). Article Google Scholar * Lv, K. _et al._ Selection of new immunotherapy targets for
NK/T cell lymphoma. _Am. J. Transl. Res._ 12(11), 7034–7047 (2020). PubMed PubMed Central Google Scholar * Lesokhin, A. M. _et al._ Nivolumab in patients with relapsed or refractory
hematologic malignancy: Preliminary results of a phase Ib study. _J. Clin. Oncol._ 34(23), 2698–2704 (2016). Article CAS Google Scholar * Sabattini, E. _et al._ WHO classification of
tumours of haematopoietic and lymphoid tissues in 2008: An overview. _Pathologica_ 102(3), 83–87 (2010). CAS PubMed Google Scholar * Cheson, B. D. _et al._ International Harmonization
Project on Lymphoma. Revised response criteria for malignant lymphoma. _J. Clin. Oncol._ 25(5), 579–586 (2007). Article Google Scholar * Kiyasu, J. _et al._ Expression of programmed cell
death ligand 1 is associated with poor overall survival in patients with diffuse large B-cell lymphoma. _Blood_ 126(19), 2193–2201 (2015). Article CAS Google Scholar * Yang, Z. Z. _et
al._ PD-1 expression defines two distinct T-cell sub-populations in follicular lymphoma that differentially impact patient survival. _Blood Cancer J._ 5, e281 (2015). Article Google Scholar
* Roncador, G. _et al._ Expression of two markers of germinal center T cells (SAP and PD-1) in angioimmunoblastic T-cell lymphoma. _Haematologica_ 92(8), 1059–1066 (2007). Article CAS
Google Scholar * Jo, J. C. _et al._ Expression of programmed cell death 1 and programmed cell death ligand 1 in extranodal NK/T-cell lymphoma, nasal type. _Ann. Hematol._ 96(1), 25–31
(2017). Article CAS Google Scholar * Muhamad, H. _et al._ Programmed cell death 1 and programmed cell death ligands in extranodal natural killer/T cell lymphoma: Expression pattern and
potential prognostic relevance. _Acta Haematol._ 143, 78–88 (2020). Article CAS Google Scholar * Chen, B. J. _et al._ PD-L1 expression is characteristic of a subset of aggressive B-cell
lymphomas and virus-associated malignancies. _Clin. Cancer Res._ 19(13), 3462–3473 (2013). Article CAS Google Scholar * Li, P. _et al._ Persistent peripheral blood EBV-DNA positive with
high expression of PD-L1 and upregulation of CD4 + CD25 + T cell ratio in early stage NK/T cell lymphoma patients may predict worse outcome. _Ann. Hematol._ 97, 2381–2389 (2018). Article
CAS Google Scholar * Bi, X. W. _et al._ PD-L1 is upregulated by EBV-driven LMP1 through NF-κB pathway and correlates with poor prognosis in natural killer/T-cell lymphoma. _J. Hematol.
Oncol._ 9(1), 109 (2016). Article Google Scholar * Wang, H. _et al._ High post-treatment serum levels of soluble programmed cell death ligand 1 predict early relapse and poor prognosis in
extranodal NK/T cell lymphoma patients. _Oncotarget_ 7(22), 33035–33045 (2016). Article Google Scholar * Kim, W. Y. _et al._ Expression of programmed cell death ligand 1 (PD-L1) in
advanced stage EBV-associated extranodal NK/T cell lymphoma is associated with better prognosis. _Virchows Arch._ 469, 581–590 (2016). Article CAS Google Scholar Download references
FUNDING This research was supported by a grant to C.X. from the Sichuan Science and Technology Program (2019YFS0027). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of
Hematology/Hematology Research Laboratory, West China Hospital, Sichuan University, #37 Guo Xue Xiang Street, Chengdu, 610041, China Yu Feng, Caixia Jing, Xinmei Yu, Yuhuan Zheng &
Caigang Xu * Department of Traditional Chinese Medicine, The Public Health Clinical Center of Chengdu, Chengdu, China Xia Feng Authors * Yu Feng View author publications You can also search
for this author inPubMed Google Scholar * Xia Feng View author publications You can also search for this author inPubMed Google Scholar * Caixia Jing View author publications You can also
search for this author inPubMed Google Scholar * Xinmei Yu View author publications You can also search for this author inPubMed Google Scholar * Yuhuan Zheng View author publications You
can also search for this author inPubMed Google Scholar * Caigang Xu View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS C.X. initiated the
project and designed the research. Y.F. and X.F. performed most experiments, analyzed the data, and drafted the manuscript. X.F. assisted in collecting clinical specimens. C.J., X.C., X.Y.,
X.F. and Y.Z. performed some experiments and provided critical suggestions. CORRESPONDING AUTHOR Correspondence to Caigang Xu. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no
competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and
reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes
were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to
obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS
ARTICLE Feng, Y., Feng, X., Jing, C. _et al._ The expression and clinical significance of programmed cell death receptor 1 and its ligand in tumor tissues of patients with extranodal nasal
NK/T cell lymphoma. _Sci Rep_ 12, 36 (2022). https://doi.org/10.1038/s41598-021-02515-5 Download citation * Received: 08 June 2021 * Accepted: 10 November 2021 * Published: 07 January 2022 *
DOI: https://doi.org/10.1038/s41598-021-02515-5 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is
not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative