Risk factors associated with neonatal mortality among neonates admitted to neonatal intensive care unit of the university teaching hospital in lusaka
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT Globally, several children die shortly after birth and many more of them within the first 28 days of life. Sub-Sharan Africa accounts for almost half (43%) of the global neonatal
death with slow progress in reduction. These neonatal deaths are associated with lack of quality care at or immediately after birth and in the first 28 days of life. This study aimed to
determine the trends and risk factors of facility-based neonatal mortality in a major referral hospital in Lusaka, Zambia. We conducted retrospective analysis involving all neonates admitted
in the University Teaching Hospital Neonatal Intensive Care Unit (UTH-NICU) in Lusaka from January 2018 to December 2019 (N = 2340). We determined the trends and assessed the factors
associated with facility-based neonatal mortality using Generalized Linear Models (GLM) with a Poisson distribution and log link function. Overall, the facility-based neonatal mortality was
40.2% (95% CI 38.0–42.0) per 1000 live births for the 2-year period with a slight decline in mortality rate from 42.9% (95% CI 40.0–46.0) in 2018 to 37.3% (95% CI 35.0–40.0) in 2019. In a
final multivariable model, home delivery (ARR: 1.70, 95% CI 1.46–1.96), preterm birth (ARR: 1.59, 95% CI 1.36–1.85), congenital anomalies (ARR: 1.59, 95% CI 1.34–1.88), low birthweight (ARR:
1.57, 95% CI 1.37–1.79), and health centre delivery (ARR: 1.48, 95% CI 1.25–1.75) were independently associated with increase in facility-based neonatal mortality. Conversely, hypothermia
(ARR: 0.36, 95% CI 0.22–0.60), antenatal attendance (ARR: 0.76, 95% CI 0.68–0.85), and 1-day increase in neonatal age (ARR: 0.96, 95% CI 0.95–0.97) were independently associated with
reduction in facility-based neonatal mortality. In this hospital-based study, neonatal mortality was high compared to the national and global targets. The improvement in neonatal survival
observed in this study may be due to interventions including Kangaroo mother care already being implemented. Early identification and interventions to reduce the impact of risks factors of
neonatal mortality in Zambia are important. SIMILAR CONTENT BEING VIEWED BY OTHERS DETERMINANTS OF EARLY NEONATAL MORTALITY (HOSPITAL BASED RETROSPECTIVE COHORT STUDY IN SOMALI REGION OF
ETHIOPIA) Article Open access 20 January 2023 NEONATOLOGIST STAFFING IS RELATED TO THE INTER-HOSPITAL VARIATION OF RISK-ADJUSTED MORTALITY OF VERY LOW BIRTH WEIGHT INFANTS IN KOREA Article
Open access 09 September 2024 SURVIVAL AND MORTALITY OF PRETERM NEONATES IN A NEONATAL INTENSIVE CARE UNIT IN NORTHERN ETHIOPIA: A RETROSPECTIVE COHORT STUDY Article Open access 12 January
2022 INTRODUCTION Neonatal mortality is the death of newborns during the first 28 days of life after a live birth. Globally, 47% of the mortality in children under-5 years are attributed to
neonatal death1,2. The burden of neonatal mortality continues to be a public health concern, especially in developing countries3. For instance, in 2019, 2.4 million neonates died globally
with sub-Saharan Africa accounting for 41% of the neonatal death1,4. The risk of neonatal mortality is thirty times higher in sub-Saharan Africa compared with the lowest neonatal mortality
in the United States2. Even though neonatal mortality estimates in sub-Saharan Africa have reduced from 45.6 deaths per 1000 livebirths in 1990 to 27.1 deaths per 1000 livebirths in 2019,
this mortality risk is still unacceptably high5,6. Several factors including sociodemographic, reproductive health, perinatal care, child-feeding practices are found to be associated with
increases in general population and facility-based neonatal mortality rates especially in developing countries. For instance, lower maternal educational levels7,8, place of delivery and
residence3,9,10, maternal age4,7,9,11, parity11, gestational age4,7,9, inadequate antenatal visits12,13, newborn sex3, newborn age14,15, mode of delivery16,17, low birthweight10,15, both
maternal and foetal complications14, preterm birth15, low Apgar score18, perinatal asphyxia19, congenital anomalies14, neonatal infections20, hypothermia21, respiratory distress syndrome20,
late initiation and or lack of exclusive breastfeeding22 are significantly associated with neonatal mortality in developing countries. Interventions addressing issues during pregnancy,
intrapartum care, nutrition, and postnatal care including proper care for small and sick newborns can significantly reduce the risk of both facility-based and general neonatal mortality. In
Zambia, neonatal mortality decreased from 37 in 2001 to 27 deaths per 1000 live births in 201823. Several strategies, policy interventions and program implementations contributed to this
progress in the neonatal mortality reduction. Programs such as helping baby breath campaign, Emergency Obstetric and Neonatal Care (EmONC) training and implementation, Saving Mothers Giving
Life (SMGL), Safe Motherhood 360 + projects, decentralization of mother and newborn care, amongst others are being implemented to reduce neonatal mortality to 12 per 1000 live births by 2030
according to the Sustainable Development Goals (SDG)3,10,19. It is important to highlight the pattern of neonatal mortality and associated risk factors especially in referral health
facilities, adding to the limited scientific evidence on the progress made and challenges. This may contribute to policy-directions in Zambia on targeted interventions towards attaining its’
neonatal mortality reduction goal by 2030. In this study, we aimed to estimate the neonatal mortality rates and investigate the risk factors associated with neonatal mortality in a major
referral health facility for targeted interventions. METHODS STUDY DESIGN AND SETTINGS This is a retrospective descriptive study using neonatal admissions records (January 1, 2018–December
31, 2019) of the Neonatal Intensive Care Unit (NICU) at the women and new-born hospital of the University Teaching Hospital (UTH), Zambia. UTH is the largest tertiary hospital which trains
all calibre of health professionals and serves as a major referral hospital in Zambia. It is located approximately four kilometres east of the city centre of the capital city of Lusaka.
STUDY PARTICIPANTS, SAMPLING PROCURE AND SAMPLE SIZE In this study, a neonate is defined as any newborn less than 28 days of life. The study population included all neonates admitted to the
NICU with complete information on required variables in the first 28 days of life at the NICU either discharge alive/death or still on admission at 28 days maximum. A complete enumeration
method was used and all reported neonates admitted to the NICU over the study period were sampled for data completeness and inclusion. The data was extracted from the neonatal case records
of the UTH-NICU health management information systems. Hard copies of individual case files were collected from the medical records and required information extracted into predesigned
excel-based data collection tool with variables of interest. The data was collected by the primary author and validated by two co-authors for completeness and accuracy. Data cleaning, coding
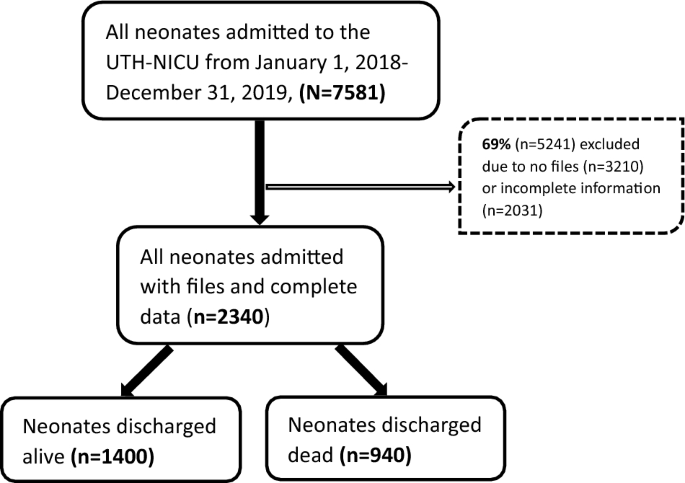
and cross-validation with the original data source was done by the researchers before it was exported into STATA version BE/18.0 for analyses. A total of 7581 neonatal admissions were
recorded during the study period. Of these, more than half (69%) were excluded (3210 missing files and 2031 incomplete data) and 31% (2340) consisting of 1197 in 2018 and 1143 in 2019 were
included in the final analyses (see Fig. 1). Assuming a minimum power of 80% using the freedom method24, the included records were sufficient enough to detect at least 8% difference in our
facility-based neonatal mortality compared with the general neonatal population mortality in Zambia with 95% precision and 5% significance level25. MEASURES The dependent (outcome) variable
was neonatal mortality among neonates admitted at the NICU which was measured as a binary outcome: died or alive at the time of discharge from the NICU or 28 days maximum. If a woman had a
live birth but lost the neonate within the first 28 days after birth it was coded as “1” or otherwise coded “0”. The independent variables included sociodemographic, maternal, and neonatal
related factors. The sociodemographic data that were captured included age of mother (years), age of neonate (days), sex of neonate, and residence. Self-reported maternal related variables
captured were parity, gravida, place of birth (hospital, health centre, and home), antenatal attendance (no, yes, and unknown), mode of delivery (spontaneous vaginal, caesarean section,
breech-assisted, and vacuum-assisted), category of staff who conducted the delivery (midwife, doctor and unskilled staff), HIV status of mother (known negative, known positive, and unknown).
Neonatal related factors included were primary diagnosis on admission to the NICU (birth asphyxia, congenital anomalies, prematurity, respiratory distress syndrome, sepsis, hypothermia,
jaundice, glycaemia, stable neonate, and other diagnosis), gestational age (weeks), and birth weight (grams). The gestational age was categorized into preterm (< 37 weeks gestation) and
term (≥ 37 weeks gestation). Birth weight was also categorized into low birth weight (< 2500 g) and normal birth weight (≥ 2500 g). STATISTICAL ANALYSIS We presented descriptive
statistics as medians and interquartile ranges (IQR) for non-normally distributed continuous variables, and frequencies with percentages for categorical variables. The Chi-square test was
used for categorical variables and Mann Whitney test for continuous variables to determine if there is significant difference in outcomes amongst the variables. To evaluate associations with
neonatal mortality, we used Poisson Regression Models to obtain incident rate ratio (IRR) along with 95% confidence Intervals (CI). We used Generalized Linear Models (GLM) with a Poisson
distribution and log link function. This is a flexible model within the GLM that assumes a linear relationship between the independent variables and binary outcome allowing logarithmic
transformation of variables to return an exposure coefficient whose natural exponents can be interpreted as risk ratios26. We applied robust variance estimator to obtain valid standard
errors which accounts for model misspecification that occurs because the binary outcome does not follow a Poisson distribution26,27. The model goodness of fit was assessed based on low
Akaike Information Criterion (AIC), and likelihood-ratio test. To identify the factors that remained independently associated with our outcome, we fitted a single multivariable Poisson
regression model that, at the outset, included all covariates and potential confounders for which a Wald test of their estimated coefficient yielded _p_ < 0.05 in the univariable
analyses. This resulted in estimation of adjusted incidence rate ratio (AIRR) with 95% CI. To test the robustness of this method, the model was repeated using automated stepwise backward
elimination procedures based on AIC. Both methods yielded the same results after adjusting for time in each model. We also stratified our analyses by gestation (preterm: < 37 weeks, term:
≥ 37 weeks) and birth weight (low birth weight: < 2500 g, normal birth weight: ≥ 2500 g) categories to determine whether these outcomes impact neonatal mortality incidence rate ratios
differently. Categorical independent variables (e.g., sex, place of birth, mode of delivery, HIV status, and antenatal attendance) were modelled as dummy variables compared to a reference
category and continuous variables as linear predictors after confirming that a linear predictor fitted well. A two-tailed (_p_ < 0.05) was considered statistically significant. STATA
version BE/18.0 was used to perform all analyses. ETHICAL APPROVAL AND CONSENT TO PARTICIPATE The University of Zambia Biomedical Research Ethics Committee (UNZBREC) approved the current
study and conforms to the 1964 Declaration of Helsinki Ethical Standards for Human Research. The informed consent was waived by UNZBREC due to the retrospective nature of the study. RESULTS
SAMPLE REPRESENTATIVENESS We compared participants included (n = 2340) and those excluded that have files but incomplete information (n = 2031) and found no significant differences by
gestational age in weeks (_p_ = 0.25), neonatal age on admission in days (_p_ = 0.42), sex (_p_ = 0.71), place of birth (_p_ = 0.32), and birthweight (_p_ = 0.19). PARTICIPANT
CHARACTERISTICS The participant characteristics shown in Table 1 indicate that the median maternal age was 25 years (IQR: 21–31), median gravida was 2 (IQR: 1–4), median parity was 2 (IQR:
1–3) and median gestation was 36 weeks (IQR: 30–37). The majority (76%) of the mothers were known to be HIV negative, and 84% of them attended antenatal care during their pregnancy. Of the
2340 neonates admitted at the NICU during the study period, the median neonatal age at admission was 4 days (IQR: 2–7) with 52% of them being males, 91% were born at the hospitals, 83% were
born via spontaneous vaginal delivery, 80% were delivered by a midwife, 69% were born preterm (< 37 weeks gestation), and 51% were low birth weight (< 2500 g). Most of the neonates
(60%) were discharged alive and 40% (940) were discharged as died. Compared to those neonates discharged alive, those neonates who were discharged as died were more likely to; be females
(51% vs. 46%, _p_ < 0.001), have lower gestational age at birth (32 weeks vs. 36 weeks, _p_ < 0.001), have short life after birth (2 days vs. 5 days, _p_ < 0.001), be born preterm
(< 37 weeks vs. ≥ 37 weeks, _p_ < 0.001) and have low birth weight (< 2500 g vs. ≥ 2500 g, _p_ < 0.001). TRENDS OF, AND FACTORS ASSOCIATED WITH, NEONATAL MORTALITY In terms of
trend, the overall neonatal mortality rate ratio (RR) was 402 (95% CI 380–420, _p_ < 0.001) per 1 000 live births for the 2-year period with a slight decline from 429 (95% CI 400–460, _p_
< 0.001) in 2018 to 373 (95% CI 350–400, _p_ < 0.001) per 1000 live births in 2019 (Table 2). Univariable analyses (Table 3) showed that, increased parity, sex, place of birth, mode
of delivery, being born preterm, lower birth weight, and primary diagnosis of congenital anomalies or prematurity were associated with increase in neonatal mortality rate ratios. In
contrast, increase in gestational age, increase in neonatal age, antenatal attendance, and primary diagnosis of sepsis, hypothermia, jaundice, glycaemia (hyper or hypo), stable neonates were
associated with decrease in neonatal mortality rate ratios. For instance, compared with those born in the hospitals, being born in the health centre and at home were significantly
associated with 46% (RR: 1.46, 95% CI 1.22–1.75) and 75% (RR: 1.75, 95% CI 1.51–2.02) increase in neonatal mortality rate ratios, respectively. Similarly, being born preterm (< 37 weeks),
having low birth weight (< 2500 g), and having a primary diagnosis of congenital anomalies after birth were significantly associated with 144% (RR: 2.44, 95% CI 2.09–2.84), 143% (RR:
2.43, 95% CI 2.16–2.73), and 69% (RR: 1.69, 95% CI 1.44–1.97) increase in neonatal mortality rate ratios, respectively. On the contrary, a 1-day increase in neonatal age, 1-week increase in
gestational age, antenatal attendance (Yes), and primary diagnosis of sepsis were significantly associated with 5% (RR: 0.95, 95% CI 0.93–0.97), 9% (RR: 0.91, 95% CI 0.90–0.92), 39% (RR:
0.61, 95% CI 0.54–0.68), and 55% (RR: 0.45, 95% CI 0.36–0.56) reduction in neonatal mortality rate ratios, respectively. In the multivariable model, being born at the health centre or home,
breech delivery, vacuum assisted delivery, being born preterm, having low birth weight, and having a primary diagnosis of congenital anomalies after birth were independently associated with
increase in neonatal mortality rate ratios. On the other hand, increase in neonatal age, antenatal attendance and primary diagnoses of respiratory distress syndrome, sepsis, hypothermia,
jaundice, glycaemia, stable neonates were also independently associated with decrease in neonatal mortality rate ratios. For example, being born at home, being born preterm, a primary
diagnosis of congenital anomalies, having low birth weight, and being born in the health centre remained independently associated with 70% (ARR: 1.70, 95% CI 1.46–1.96), 59% (ARR: 1.59, 95%
CI 1.36–1.85), 59% (ARR: 1.59, 95% CI 1.34–1.88), 57% (ARR: 1.57, 95% CI 1.37–1.79), and 48% (ARR: 1.48, 95% CI 1.25–1.75) increase in neonatal mortality rate ratios, respectively.
Conversely, primary diagnosis of hypothermia, antenatal attendance (yes), and one-day increase in neonatal age were independently associated with 64% (ARR: 0.36, 95% CI 0.22–0.60), 24% (ARR:
0.76, 95% CI 0.68–0.85,), and 4% (ARR: 0.96, 95% CI 0.95–0.97) reduction in neonatal mortality rate ratios, respectively. ASSOCIATIONS WITH NEONATAL MORTALITY STRATIFIED BY GESTATIONAL AGE
AND BIRTH WEIGHT The strength of the association varies by gestational age at birth and birth weight in the univariable stratified analyses (Tables 4 and 5). While sex, antenatal attendance,
and low birth weight associations with neonatal mortality rate ratios were stronger for neonates born preterm (< 37 weeks gestation), stronger associations were observed with congenital
anomalies, mode of delivery and increase age of neonates for those neonates born at term (≥ 37 weeks gestation). A similar pattern of associations with neonatal mortality rate ratios were
observed for birth weight. For instance, 1-day increase in age of neonate, mode of delivery, congenital anomalies, and antenatal attendance were strongly associated with neonatal mortality
rate ratios for neonates born with normal birth weight (≥ 2500 g) while only sex and being born preterm were strongly associated with neonatal mortality rate ratios for neonates with low
birth weight (< 2500 g). In the multivariable analyses (Table 4), several factors including age of neonate, antenatal attendance, vacuum delivery, being delivered at health centre,
congenital anomalies, respiratory distress, sepsis, hypothermia were independently associated with neonatal mortality rate ratios in both preterm and term neonates. Interestingly, being born
at health centre and home, breech-assisted and vacuum delivery, and low birth weight were independently associated with increase in neonatal mortality rate ratios in preterm neonates. In
Table 5, similar several common factors including age of neonate, antenatal attendance, breech delivery, being deliver at health centre, congenital anomalies, jaundice, and being born
preterm were independently associated with neonatal mortality rate ratios in both normal weight and low birth weight neonates. However, caesarean-section, breech-assisted and vacuum-assisted
delivery as well as respiratory distress syndrome, sepsis, hypothermia, and glycaemia were independently associated with neonatal mortality rate ratios in neonates with low birth weight.
DISCUSSION In this study, we examined the trends and determinants of neonatal mortality of neonates admitted to the women and new-born tertiary hospital in Lusaka, Zambia between 2018 and
2019. Overall, we found that 40% (402/100,000 live births) of neonates admitted to the NICU died over the 2-years period with a 6% (56/100,000 live births) slight decline from 2018 to 2019.
Being born at health centre and home, breech and vacuum modes of delivery, preterm birth, low birth weight and congenital anomalies were independently associated with increase in neonatal
mortality. On the contrary, increase in neonatal age, antenatal attendance and primary diagnosis of respiratory distress, sepsis, hypothermia, jaundice, glycaemia, and stable neonates were
independently associated with decrease in neonatal mortality. These associations were generally stronger for neonates born preterm or with low birthweight compared to neonates born at term
or with normal birthweight. These findings are important and seem to suggest that efforts at increasing skilled birth at health facility or home, early interventions in reducing
pregnancy/birth complications, and other adverse birth outcomes are still vital in reducing neonatal mortality rates. Contrary to our expectations, we found a higher cumulative neonatal
mortality over the 2-years period, with a gradual decrease in trend from 2018 to 2019 in a higher level of referral system where high quality of care and expertise are expected. These rates
are much higher than the general national neonatal mortality rates of 32/1000 live births in 2018 and 33/1000 in 201928,29. The UTH-NICU in Lusaka receives major referrals across the country
and from surrounding communities and it is possible that most neonates referred to the facility were in critical condition and therefore were subject to low survival rates. In addition,
there may be delays in or inappropriate obstetric referrals from lower-level health facilities suggesting that late arrivals for life-saving interventions, overwhelmed referral facilities or
lack of timely comprehensive obstetric care may have compromised quality of care and consequently reduced neonatal survival rates. These may have accounted for the high neonatal mortality
rates observed in this study. Considering that Lusaka alone contributes 19% of the country’s total population and that Zambia is one of the countries with higher urban than rural neonatal
mortality rates4, efforts to improve neonatal health outcomes in Lusaka may significantly contribute to the reduction of neonatal mortality in the country. We found that several factors were
associated with increase in neonatal mortality. For example, being born at home, or health centre compared with hospital, breech and vacuum delivery compared with spontaneous vaginal were
associated with 70%, 48%, 69%, and 39%, increase in neonatal mortality rates, respectively. Similar to our findings, home and health centre delivery were found to be significant risk factors
for neonatal mortality in Africa including Zambia8. Lower maternal education, inability to pay for cost of care at the hospital, health care worker attitudes, religious beliefs, long travel
distance and lack of husband approval were some of the factors attributable to home delivery8. Previous studies in Ethiopia30,31,32, Benin16, and Eretria18 also found breech and vacuum
deliveries to be significant risk factors for neonatal mortality in neonates referred to NICUs. Continual education of health care workers especially nurses and midwives in emergency
obstetric care, timely risks assessment and timely referral of high-risk expectant mothers, improved breech and vacuum deliveries procedure and management, and neonatal resuscitation may
contribute to the reduction of neonatal mortality3,14. In addition, appropriate education of expectant mothers empathizing regular antenatal visits, early birth preparedness involving their
husbands, and health facility deliveries may assist mothers to have safe deliveries and reduce neonatal mortality3,14. Improvement in community and health centre level referral systems to
reduce transport delays and establishment of functional mothers’ shelter near health facilities may assist those far away to have easy and early access to referral sites for appropriate
interventions that may contribute to a reduction in neonatal mortality3,14. In addition, we found congenital anomalies to be associated with 59% increased risk of neonatal mortality in our
study with stronger effect sizes observed in preterm and low birthweight neonates. The global incidence of congenital anomalies is about 3–4% in all births. Globally, congenital anomalies
are the fourth leading cause of neonatal mortality with an annual death of 240,000 of which 90% with serious disorders are from low-and-middle-income countries33. Our findings are similar to
previous studies in Nigeria34, Ghana35, and South Africa36 where congenital anomalies was found to have accounted for 10.4–33.5% of neonatal mortality of neonates admitted to NICU. Measures
to promote primary prevention and improve the health of neonates with congenital disorders via improved surveillance, building capacity and increase expertise on prevention and care,
increasing awareness on newborn screenings, strengthening research on major birth defects, and supporting affected families may help reduce the burden of congenital anomalies33. Predictably,
we found that antenatal attendance was associated with 24% decrease in neonatal mortality. Similarly, previous survival analysis of risk factors of neonatal mortality in low-middle-income
countries indicated that one antenatal attendance lowers the risk of neonatal mortality by 26% and this increased to 51% lower risk if the antenatal visits are up to four37. A recent
meta-analysis also highlighted that less than four antenatal visits increase the risk of neonatal mortality by 1.76 times compared to those that had four antenatal visits38. Adequate
antenatal visits are important to help in early detection and appropriate management of birth-related problems to reduce pregnancy/birth complication and the risk of neonatal death.
Interestingly, we found that primary diagnosis of glycaemia (hypoglycaemia and hyperglycaemia), hypothermia, jaundice, sepsis, and respiratory distress syndrome were associated with 65%,
64%, 59%, 51%, and 25% decrease in neonatal morality, respectively. These are important findings and highlights that measures implemented by the Zambia government and its partners to address
common preventable neonatal death in the health facilities appears to be yielding the expected outcomes. Several strategic policy and implementation-related decisions were made between 2000
and 2017 in areas of capacity building of health care workers, healthcare infrastructure improvement, increase availability of skilled birth attendance, and community outreach programs to
encourage facility level delivery. Implementation of key strategic programs such as maternal and perinatal death review, essential newborn care, Kangaroo mother care, helping babies breathe,
Safe Motherhood practices, and interventions using the EmONC recommendations may have contributed significantly to the reduction of preventable neonatal death observed in this study3,39. In
general, associations with neonatal mortality were stronger for preterm (< 37 weeks gestation) than for term neonates (≥ 37 weeks gestation) and were also stronger for low birthweight
(< 2500 g) compared to normal birthweight (≥ 2500 g) neonates. The finding of stronger associations for preterm is consistent with a meta-analysis which found that preterm birth
consistently accounted for 5.7–7.1 times higher neonatal mortality rates than term birth40. Similarly, the same meta-analysis found low birth weight to have consistently accounted for
9.9–15.5 times higher neonatal mortality rates compared to normal birthweight40. This implies that interventions targeting improve care for preterm and low birthweight neonates may reduce
neonatal mortality. The findings of this study should be interpreted taking into consideration its’ limitations. We could not retrieve all case files of neonates admitted at the NICU and
amongst those retrieved, many had inadequate information of maternal and perinatal characteristics. Those neonates who died on arrival or who were not registered in the NICU register were
not captured. Selection bias may have occurred as not all neonate admitted were included. When we compared this study participants to those not included but have limited information, there
were no differences in gestational age, age of neonates on admission, sex, place of birth and birthweight. We further examined whether gestational age, age of neonate on admission, sex,
place birth and birthweight confounded our relationships but this was not the case. This supports the view that population differences may affect prevalence estimates but are not likely to
substantially affect exposure-outcome relationships41. Nonetheless, considering that this is a hospital-based retrospective study, the findings cannot be generalizable to the general
neonatal population. Despite this, the study highlights the trends and determinants of neonatal morality in a major referral centre in the country which is important for policy
interventions. CONCLUSION Neonatal mortality in a major referral centre in Zambia highlights a slight reduction between 2018 and 2019 implying that current efforts towards achieving the
neonatal mortality SDG goal is gradually being achieved. The findings of our study indicate that some of the factors associated with neonatal mortality especially in the NICU are being
successfully implemented by the government of Zambia. It is therefore important to continue with the improvement in prenatal and intrapartum care, obstetric emergency services, and postnatal
care geared towards the reduction of neonatal mortality in Zambia. It is also important to continue to monitor the trends and cause-specific neonatal mortality at all levels especially in
referral hospitals as well as rural urban disparities to support improve quality of care and key decision-making. Our study findings provide important information and pointers to guide
Government and partners in identifying and prioritizing key neonatal mortality problems in their health policy development and interventions. DATA AVAILABILITY The datasets used in this
current study is available from the corresponding author on reasonable request. ABBREVIATIONS * AIC: Akaike information criterion * EmONC: Emergency obstetric and neonatal care * FETP: Field
Epidemiology Training Program * HMIS: Health management information system * MOH: Ministry of Health * NICU: Neonatal intensive care unit * NMR: Neonatal mortality rate * SDGs: Sustainable
Developmental Goals * UTH: University Teaching Hospital REFERENCES * World Health Organisation. Newborn Mortality. (2022).
https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-mortality-report-2021 Accessed 14 Sept 2023. * Hug, L. _et al._ National, regional, and global levels and trends
in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: A systematic analysis. _Lancet Glob. Health_ 7(6), e710–e720 (2019). Article PubMed PubMed Central
Google Scholar * Kamanga, A. _et al._ Reducing maternal and neonatal mortality through integrated and sustainability-focused programming in Zambia. _PLoS Global Public Health_ 2(12),
e0001162 (2022). Article PubMed PubMed Central Google Scholar * Norris, M. _et al._ A growing disadvantage of being born in an urban area? Analysing urban–rural disparities in neonatal
mortality in 21 African countries with a focus on Tanzania. _BMJ Glob. Health_ 7(1), e007544 (2022). Article PubMed PubMed Central Google Scholar * Akombi, B. J. & Renzaho, A. M.
Perinatal mortality in sub-Saharan Africa: A meta-analysis of demographic and health surveys. _Ann. Global Health_ 85(1) (2019). * Tekelab, T. _et al._ The impact of antenatal care on
neonatal mortality in sub-Saharan Africa: A systematic review and meta-analysis. _PLoS ONE_ 14(9), e0222566 (2019). Article PubMed PubMed Central CAS Google Scholar * Kc, A. _et al._
Trends for neonatal deaths in Nepal (2001–2016) to project progress towards the SDG target in 2030, and risk factor analyses to focus action. _Matern. Child Health J._ 24, 5–14 (2020).
Article PubMed Google Scholar * Grady, S. C., Frake, A. N., Zhang, Q., _et al._ Neonatal mortality in East Africa and West Africa: A geographic analysis of district-level demographic and
health survey data. _Geospat. Health _12(1) (2017). * Guinsburg, R. _et al._ Annual trend of neonatal mortality and its underlying causes: Population-based study–São Paulo State, Brazil,
2004–2013. _BMC Pediatr._ 21(1), 1–9 (2021). Article Google Scholar * Yang, Y., Patterson, A. & Yimer, B. E. Cost-effectiveness comparison of the ReMiND program and the Newhints
program for reducing neonatal mortality rates in the Muchinga Province of Zambia. _Public Health Rev._ 4(2) (2021). * Kujala, S. _et al._ Trends and risk factors of stillbirths and neonatal
deaths in Eastern Uganda (1982–2011): A cross-sectional, population-based study. _Trop. Med. Int. Health_ 22(1), 63–73 (2017). Article PubMed Google Scholar * Saloio, C. Á., Neto OLd, M.,
Gonçalves, D.A., _et al._ Magnitude and determinants of neonatal and postneonatal mortality in Goiânia, Goiás, Brazil: a retrospective cohort study, 2012. _Epidemiol. Serv. Saúde_ 29
(2020). * Kibret, G. D., Demant, D. & Hayen, A. The effect of distance to health facility on neonatal mortality in Ethiopia. _BMC Health Serv. Res._ 23(1), 114 (2023). Article PubMed
PubMed Central Google Scholar * Miyoshi, Y. _et al._ Baby survival in Zambia: Stillbirth and neonatal death in a local hospital setting. _BMC Pregn. Childbirth_ 19(1), 1–6 (2019). Article
Google Scholar * Saleem, S. _et al._ Neonatal deaths in infants born weighing ≥ 2500 g in low and middle-income countries. _Reprod. Health_ 17(2), 1–14 (2020). Google Scholar * Houssou,
M., Hessou, Y., Sawadogo, B., _et al._ Neonatal mortality and risk factors in the University Hospital of the Mother and Child Lagoon in Cotonou, Benin, 2015–2016. _J Interv Epidemiol Public
Health_ 3 (2020). * Adewuyi, E. O. & Zhao, Y. Determinants of neonatal mortality in rural and urban Nigeria: Evidence from a population-based national survey. _Pediatr. Int._ 59(2),
190–200 (2017). Article PubMed Google Scholar * Andegiorgish, A. K. _et al._ Neonatal mortality and associated factors in the specialized neonatal care unit Asmara Eritrea. _BMC Public
Health_ 20, 1–9 (2020). Article Google Scholar * Gill, C. J., Phiri-Mazala, G., Guerina, N. G., _et al._ Effect of training traditional birth attendants on neonatal mortality (Lufwanyama
Neonatal Survival Project): Randomised controlled study. _BMJ_ 342 (2011). * Turnbull, E. _et al._ Causes of stillbirth, neonatal death and early childhood death in rural Zambia by verbal
autopsy assessments. _Trop. Med. Int. Health_ 16(7), 894–901 (2011). Article PubMed PubMed Central Google Scholar * Shiferaw, K. _et al._ Neonatal mortality rate and its determinants: A
community-based panel study in Ethiopia. _Front. Pediatr._ https://doi.org/10.3389/fped.2022.875652 (2022). Article PubMed PubMed Central Google Scholar * Mitiku, H. D. Neonatal
mortality and associated factors in Ethiopia: A cross-sectional population-based study. _BMC Women’s Health_ 21(1), 1–9 (2021). Article Google Scholar * United Nations Inter-agency Group
for Child Mortality Estimation. Noenatal mortality rate for Zambia 2018. https://childmortality.org/data/Zambia Accessed 14 Sept 2023. * Freedman, L. S. Tables of the number of patients
required in clinical trials using the logrank test. _Stat. Med._ 1(2), 121–129 (1982). Article PubMed CAS Google Scholar * Mukosha, M., Kaonga, P., Kapembwa KM, et al. Modelling
mortality within 28 days among preterm infants at a tertiary hospital in Lusaka, Zambia: A retrospective review of hospital-based records. _Pan Afr. Med. J. _39(1) (2021). * Holmberg, M. J.
& Andersen, L. W. Estimating risk ratios and risk differences: Alternatives to odds ratios. _JAMA_ 324(11), 1098–1099 (2020). Article PubMed Google Scholar * Naimi, A. I. &
Whitcomb, B. W. Estimating risk ratios and risk differences using regression. _Am. J. Epidemiol._ 189(6), 508–510 (2020). Article PubMed Google Scholar * United Nations International
Children’s Emergency Fund. UN inter-agency group for child mortality estimation. _Levels Trends Child Mortality_ 2018–2019. * McClure, E. M. _et al._ The Global Network Maternal Newborn
Health Registry: A multi-country, community-based registry of pregnancy outcomes. _Reprod. Health_ 17, 1–11 (2020). Article Google Scholar * Orsido, T. T., Asseffa, N. A. & Berheto, T.
M. Predictors of Neonatal mortality in Neonatal intensive care unit at referral Hospital in Southern Ethiopia: A retrospective cohort study. _BMC Pregn. Childbirth_ 19, 1–9 (2019). Article
Google Scholar * Mohamed, H. A. _et al._ Neonatal mortality and associated factors among neonates admitted to neonatal intensive care unit at public hospitals of Somali Regional State,
Eastern Ethiopia: A multicenter retrospective analysis. _PLoS ONE_ 17(5), e0268648 (2022). Article PubMed PubMed Central CAS Google Scholar * Gudayu, T. W., Zeleke, E. G. & Lakew,
A. M. Time to death and its predictors among neonates admitted in the intensive care unit of the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. _Res. Rep.
Neonatol._ 1–10. (2020). * World Health Organisation. Congenital disorders Key facts. 2023. https://www.who.int/news-room/fact-sheets/detail/birth-defects Accessed 07 Nov 2023. * Ajao, A. E.
& Adeoye, I. A. Prevalence, risk factors and outcome of congenital anomalies among neonatal admissions in OGBOMOSO Nigeria. _BMC Pediatr._ 19(1), 1–10 (2019). Article Google Scholar *
Anane-Fenin, B., Opoku, D. A. & Chauke, L. Prevalence, pattern, and outcome of congenital anomalies admitted to a neonatal unit in a low-income country—a ten-year retrospective study.
_Matern. Child Health J._ 27(5), 837–849 (2023). Article PubMed PubMed Central Google Scholar * Malherbe, H. L. _et al._ The contribution of congenital disorders to child mortality in
South Africa. _South African Health Rev._ 2016(1), 137–152 (2016). Google Scholar * Doku, D. T. & Neupane, S. Survival analysis of the association between antenatal care attendance and
neonatal mortality in 57 low-and middle-income countries. _Int. J. Epidemiol._ 46(5), 1668–1677 (2017). Article PubMed PubMed Central Google Scholar * Belachew, A., Tewabe, T. &
Dessie, G. Neonatal mortality and its association with antenatal care visits among live births in Ethiopia: A systematic review and meta-analysis. _J. Matern-Fet. Neonat. Med._ 35(2),
348–355 (2022). Article Google Scholar * Muttau, N. _et al._ Strengthening Kangaroo Mother Care at a tertiary level hospital in Zambia: A prospective descriptive study. _PLoS ONE_ 17(9),
e0272444 (2022). Article PubMed PubMed Central CAS Google Scholar * Veloso, F. C. S. _et al._ Analysis of neonatal mortality risk factors in Brazil: a systematic review and
meta-analysis of observational studies. _J. Pediatr._ 95, 519–30 (2019). Article Google Scholar * Mealing, N. M. _et al._ Investigation of relative risk estimates from studies of the same
population with contrasting response rates and designs. _BMC Med. Res. Methodol._ 10, 1–12 (2010). Article Google Scholar Download references ACKNOWLEDGEMENTS We appreciate the support of
the Ministry of health-Zambia, monitoring, and evaluation department staff for assisting with the sampling procedures. We also thank the University teaching hospital management for granting
us permission to access the data for this research purpose. Special thanks to the staff of the neonatal Intensive Care Unit at the women and new-born hospital for the support in acquiring
the data. Finally, we appreciate the mothers and babies who contributed data to support this study. DISCLAIMERS The named authors stated here alone are responsible for the views expressed in
this publication. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of WHO concerning the
legal status of any country, territory, city, or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or of certain
manufacturers’ products does not imply that they are endorsed or recommended by WHO in preference to others of a similar nature that are not mentioned. All reasonable precautions have been
taken by WHO to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The
responsibility for the interpretation and use of the material lies with the reader. In no event shall WHO be liable for damages arising from its use. FUNDING DT undertook this study as part
of a master’s in public health and biostatistics and Field Epidemiology Training Program (FETP). The study was not funded by any organisation. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS *
School of Public Health, Department of Epidemiology and Biostatistics, University of Zambia, Lusaka, Zambia Deborah Tembo, Patrick Kaonga & Choolwe Jacobs * Zambia National Public Health
Institute, Lusaka, Zambia Deborah Tembo * World Health Organization Country Office, Maseru, Lesotho Francis D. N. Abobo * World Health Organization Country Office, Lusaka, Zambia Barnabas
Bessing Authors * Deborah Tembo View author publications You can also search for this author inPubMed Google Scholar * Francis D. N. Abobo View author publications You can also search for
this author inPubMed Google Scholar * Patrick Kaonga View author publications You can also search for this author inPubMed Google Scholar * Choolwe Jacobs View author publications You can
also search for this author inPubMed Google Scholar * Barnabas Bessing View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS D.T.: Contributed to
study conceptualisation, design, methodology, data analysis and interpretation, original draft, review, and editing. F.D.N.A.: Contributed to critical review and editing of draft. P.K. and
C.J. contributed to the study design, interpretation, and supervision of the study. B.B.: Contributed to study conceptualisation, design, methodology, data analysis and interpretation,
original draft, review, editing, and supervision of the manuscript for publication. All authors read and approved final manuscript. No individual participants identifiable data or images or
specimens is included in this study and therefore informed consent for publication is not applicable. CORRESPONDING AUTHOR Correspondence to Deborah Tembo. ETHICS DECLARATIONS COMPETING
INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and
institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing,
adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons
licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise
in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the
permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and
permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Tembo, D., Abobo, F.D.N., Kaonga, P. _et al._ Risk factors associated with neonatal mortality among neonates admitted to neonatal intensive
care unit of the University Teaching Hospital in Lusaka. _Sci Rep_ 14, 5231 (2024). https://doi.org/10.1038/s41598-024-56020-6 Download citation * Received: 20 November 2023 * Accepted: 29
February 2024 * Published: 04 March 2024 * DOI: https://doi.org/10.1038/s41598-024-56020-6 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get
shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * Neonates
mortality * NICU * Risks factors * Trends * Zambia