Differences in outcomes of patients with out-of-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation between day-time and night-time
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

Although patients who underwent night-time resuscitation for out-of-hospital cardiac arrest (OHCA) had worse clinical outcomes than those who underwent day-time resuscitation, the
differences between the outcomes of patients with OHCA who underwent extracorporeal cardiopulmonary resuscitation (ECPR) in the day-time and night-time remain unclear. We analyzed data from
the Study of Advanced Life Support for Ventricular Fibrillation with Extracorporeal Circulation in Japan. Patients were categorized according to whether they received treatment during the
day-time or night-time. The primary outcomes were survival to hospital discharge and favorable neurological outcome at discharge, and the secondary outcomes were estimated low-flow time,
implementation time of ECPR, and complications due to ECPR. A multivariate logistic regression model adjusted for confounders was used for comparison. Among the 1644 patients, the night-time
patients had a significantly longer ECMO implementation time and estimated low-flow time than the day-time patients, along with a significantly higher number of complications than the
day-time patients. However, the survival and neurologically favorable survival rates did not differ significantly between the groups. Thus, although patients who underwent ECPR at night had
an increased risk of longer implementation time and complications, their clinical outcomes did not differ from those who underwent day-time ECPR.
Out-of-hospital cardiac arrest (OHCA) is a major public health problem worldwide with a high mortality rate1,2. In Japan, emergency medical services attend to > 120,000 patients with OHCA
each year, and the 1-month survival rate of patients with OHCA was only 6–7% in recent years3, despite improvements in cardiopulmonary resuscitation (CPR) skills and widespread availability
of automated external defibrillators (AED) among the general population3,4.
Patients who underwent night-time resuscitation for OHCA had worse outcomes than those who underwent day-time resuscitation5,6,7, possibly because of compromised alertness and performance of
medical staff during night-time shifts, as well as the reduced number of medical staff members during night-time compared with day-time shifts8.
Extracorporeal cardiopulmonary resuscitation (ECPR) is an advanced emergency rescue therapy for patients with OHCA who do not achieve a return of spontaneous circulation (ROSC) in the
emergency department (ED). Patients with OHCA who underwent ECPR had better outcomes than those who received traditional resuscitation8,9,10,11,12,13,14. However, considering that ECPR
requires many human and healthcare resources, night-time ECPR could lead to worse outcomes, longer ECMO implementation durations, more complications related to ECMO cannulation, and a lower
survival rate than day-time ECPR. Although the differences in the characteristics and clinical outcomes among in-hospital cardiac arrest (IHCA) patients who underwent ECPR by treatment time
have previously been reported15, the differences among OHCA patients remain uninvestigated. Considering that differences in the quality of resuscitation can be influenced by prehospital
circumstances, OHCA patients might have more differences in outcomes based on when the ECPR occurred. Therefore, we assessed the implementation time-related differences in clinical
characteristics and outcomes in patients with OHCA treated with ECPR.
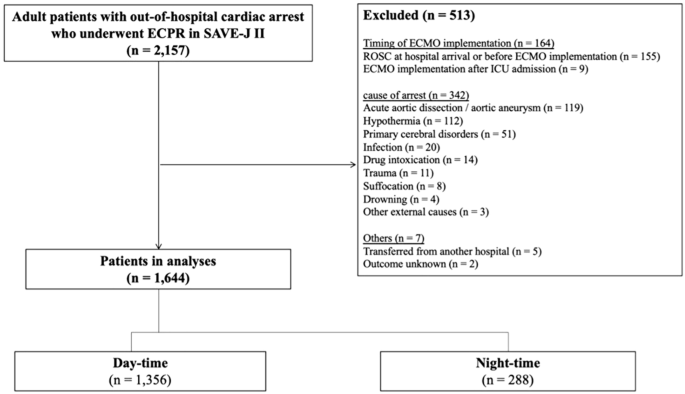
We analyzed data from the Study of Advanced Life Support for Ventricular Fibrillation with Extracorporeal Circulation in Japan (SAVE-JII study)16, a retrospective large multicenter registry
study that examined the effectiveness of ECPR on clinical outcomes in Japan between January 1, 2013, and December 31, 2018.
This study was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN000036490). The study protocol was approved by the ethics committee of Tokyo
Medical and Dental University Hospital (M2019-018) and all research was performed in accordance with relevant regulations. The requirement for informed consent was waived in all the
participating institutions by the ethics committee of Tokyo Medical and Dental University Hospital because of the retrospective nature of the study.
Twenty-four hours a day for ECPR were available in all facilities that participated in this study, and over 90% of facilities had emergency physicians working around the clock.
Cardiologists, cardiovascular surgeons, and radiologists were available 24 h a day at 52.8%, 14.7%, and 3.0% of facilities, respectively16.
Regarding ECMO implementation, ultrasonography was used to check the site of ECMO catheter insertion and the position of the guidewire at the inferior vena cava. The positioning of the ECMO
catheter was checked by X-ray before ECMO pump-on and/or CT scan after ECMO pump-on.
The inclusion criteria were as follows: (1) patients aged ≥ 18 years and (2) patients with OHCA treated with ECPR. We excluded patients who met at least one of the following criteria: (1)
transfer to a participating institution after receiving treatment in another hospital; (2) denial to participate in the study through their family or other agents; (3) implementation of ECPR
after ROSC and/or after intensive care unit (ICU) admission; (4) the etiology of non-cardiac arrest was aortic dissection, hypothermia, primary cerebral disorder, infection, drug
intoxication, trauma, suffocation, or drowning; and, (5) missing data for survival at hospital discharge or neurological outcomes at hospital discharge.
The following data on patient characteristics, prehospital information, time course, complications, and outcomes were collected from the SAVE-J II study data: age, sex, year of admission,
incidence of witnessed cardiac arrest (CA) and bystander CPR, initial cardiac rhythm, etiology of CA, CA due to acute coronary syndrome (ACS), location of CA, center volume, complications of
ECPR implementation, survival rate at hospital discharge, and neurological outcomes at hospital discharge. Missing data other than for primary outcomes were deleted in each analysis.
Indications for ECPR followed those established by each institution. Based on previous studies, day-time was 7:00–22:59, and night-time was defined as 23:00–6:596,7,17. Initial shockable
rhythm was defined as ventricular fibrillation and pulseless ventricular tachycardia. ACS was diagnosed by coronary angiography. With respect to center volume, a high-volume center was
defined as an institution performing more than 20 cases of ECPR for OHCA patients per year, while a low-volume center was defined as performing 19 or fewer cases per year, based on previous
studies18,19 Estimated low-flow time was defined as the interval from emergency medical services (EMS) dispatch to ECMO pump-on in cases with bystander CPR or from EMS arrival to ECMO
pump-on in cases without bystander CPR. ECMO implementation time was defined as the duration from ED arrival to ECMO pump-on. ECMO complications were defined as cannulation site bleeding
and/or hematoma, retroperitoneal hematoma due to cannulation failure, and ECMO catheter malpositioning. ECMO catheter malpositioning was defined as cannulation of the wrong vessel, requiring
repositioning or reinsertion of the catheter. Interventions for cannulation-site bleeding and retroperitoneal hematoma were defined as hemostasis achieved through surgical or endovascular
treatment.
We defined primary outcomes as survival to hospital discharge and favorable neurological outcomes at discharge. A favorable neurological outcome was defined as a cerebral performance
category (CPC) score of 1 or 220.
Secondary outcomes were defined as estimated low-flow time, ECMO implementation time, and complications due to ECMO implementation.
We divided the enrolled patients into two groups by time of ECMO implementation: the day-time and night-time groups. In the univariate analysis, we used the Student’s t-test or Mann–Whitney
U test to compare continuous variables and the χ2 or Fisher exact test to compare categorical variables, as appropriate. Categorical variables were reported as numbers and percentages,
whereas continuous variables were reported as medians and interquartile ranges (IQR). Univariable and multivariable logistic regression models were used to assess the primary and secondary
outcomes. We incorporated age, sex, witnessed cardiac arrest, bystander CPR, initial shockable cardiac rhythm, diagnosis of ACS, estimated low-flow time, and night-time occurrence into the
multivariate model to assess primary outcomes. These variables were selected a priori and were clinically plausible and well-known confounders. To assess secondary outcomes in the
multivariate model, we incorporated year of admission, use of ultrasound machines, ECMO implementation in the ER, center volume, and night-time occurrence. These variables were incorporated
into the multivariate model of the secondary outcomes based on the results of the univariate analysis (cutoff: p